Bioequivalence: What It Means for Generic Drugs and Your Health
When you pick up a generic pill, you want to know it will do the same job as the brand-name version. That’s where bioequivalence, the scientific standard that proves two drug formulations release the same amount of active ingredient into the bloodstream at the same rate. Also known as pharmaceutical equivalence, it’s the invisible guarantee that your $5 generic works just like the $50 name-brand pill. Without bioequivalence, generic drugs would be little more than lookalikes—empty shells with no real therapeutic power.
Bioequivalence isn’t just a buzzword. It’s a measurable, regulated process. The FDA and global health agencies require generic manufacturers to prove their versions match the original in drug absorption, how quickly and completely the active ingredient enters your bloodstream. This isn’t about pills dissolving at the same speed in water—it’s about blood concentration curves in real people. If the generic’s absorption rate falls outside a strict 80–125% range compared to the brand, it doesn’t get approved. That’s why you don’t see random generics on shelves. Every approved one has passed this test.
And it’s not just about cost. Bioequivalence keeps you safe. A drug that absorbs too slowly might not control your blood pressure. One that floods your system too fast could cause side effects. That’s why bioequivalence studies often involve healthy volunteers who take both versions under controlled conditions, then get their blood drawn over hours. The data is plotted, compared, and verified. No guesswork. No shortcuts. This is why you can trust a generic for high-stakes meds like blood thinners, seizure drugs, or thyroid hormones.
Some people still worry generics are "weaker"—but that’s a myth built on confusion. Bioequivalence doesn’t mean identical in every way. Fillers, colors, or coatings can differ. But the active ingredient? The release profile? The final effect in your body? Those are locked in. If your doctor switches you from Lipitor to atorvastatin, or from Synthroid to levothyroxine, it’s because the science says it’s the same. And if you’ve ever noticed a change after switching? That’s often psychological—or maybe your body just needed time to adjust. True bioequivalence means the difference is negligible.
Behind every generic you take, there’s a stack of clinical data proving it works. That’s the power of bioequivalence. It’s not marketing. It’s math. It’s biology. It’s regulation. And it’s why millions of people save hundreds a year without sacrificing health. Below, you’ll find real-world examples of how this science plays out—from insurance coverage of generics to the delays in bringing them to market, and even how Indian manufacturers meet global bioequivalence standards. These aren’t abstract concepts. They’re the quiet rules that keep your prescriptions safe, affordable, and effective.
How to Compare Dissolution Profiles and What They Mean for Generic Drugs
Learn how dissolution profiles are used to prove generic drugs work like brand-name versions. Understand the f2 factor, regulatory standards, and why this test saves time and money without compromising safety.
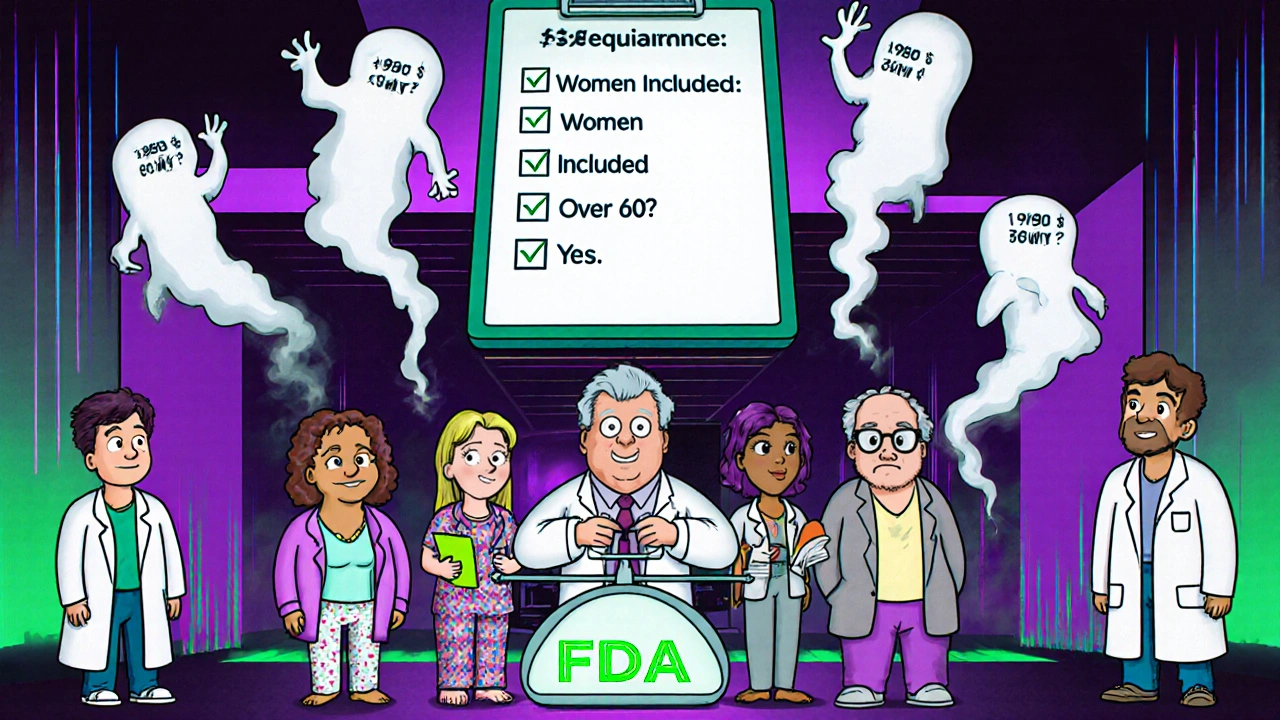
Bioequivalence Studies and the Critical Role of Age and Sex in Study Design
Bioequivalence studies must now include balanced representation of men and women, and older adults, to ensure generic drugs work safely for everyone. Regulatory agencies are updating guidelines to reflect real-world use.