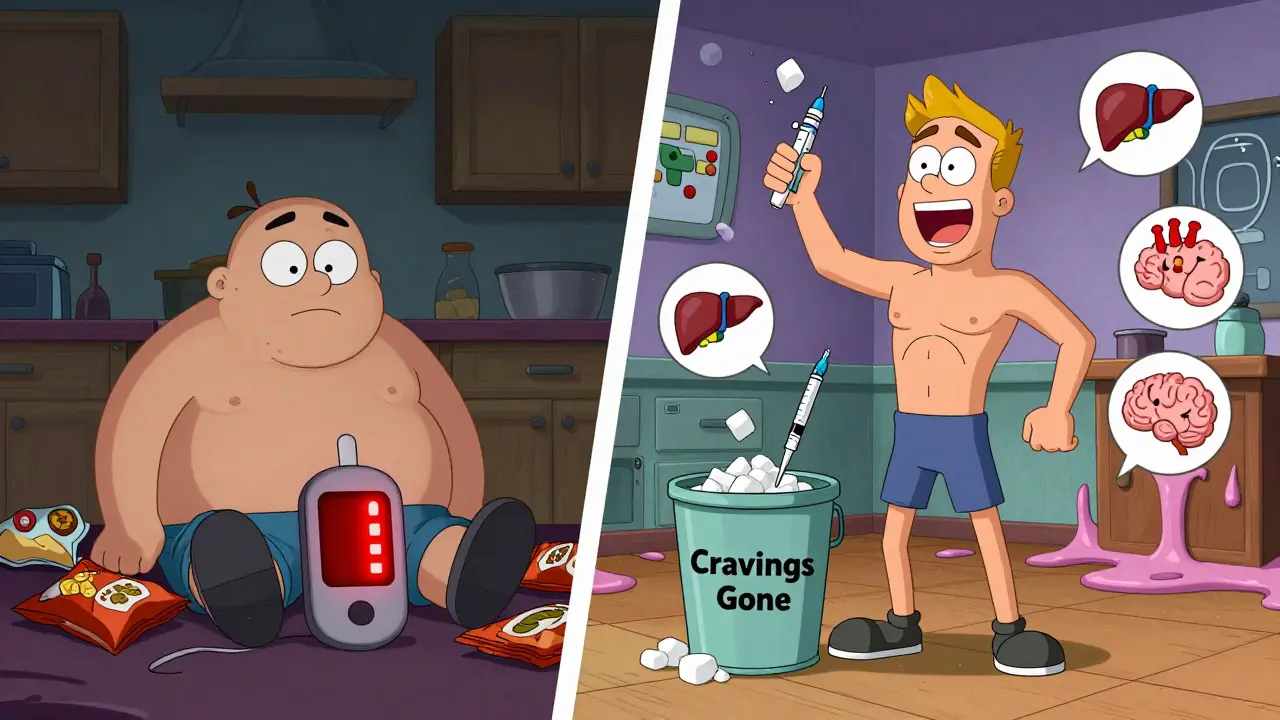
For people struggling with type 2 diabetes and excess weight, the old choices felt like a trade-off: lower blood sugar meant gaining weight, or losing weight meant juggling insulin shots and constant hunger. That’s changing. GLP-1 receptor agonists are no longer just diabetes meds-they’re turning the script on metabolic health. These injections don’t just help control blood sugar; they help you lose significant weight, often without feeling starving. And the data backs it up.
How GLP-1 Receptor Agonists Actually Work
GLP-1 is a hormone your body makes after eating. It tells your pancreas to release insulin only when blood sugar rises-no overproduction, no crashes. It also slows down how fast food leaves your stomach and sends a clear signal to your brain: ‘You’re full.’
GLP-1 receptor agonists are synthetic versions of this hormone. They mimic its actions but last longer. That means one injection a week can keep your body feeling full, your blood sugar steady, and your appetite quiet.
Here’s how it breaks down:
- Slows digestion: Food takes 15-30% longer to leave your stomach. That means no sugar spikes after meals.
- Boosts insulin: Your pancreas releases more insulin-but only when glucose is high. This reduces the risk of low blood sugar.
- Blocks glucagon: This hormone tells your liver to dump sugar into your blood. GLP-1 drugs cut that signal by 20-30%.
- Resets your appetite: In the hypothalamus, these drugs turn down hunger signals (NPY and AgRP) and turn up fullness signals (POMC/CART). Studies show hunger drops by 30-40%.
It’s not magic. It’s biology, amplified. And it’s why people on these drugs aren’t just losing weight-they’re losing cravings.
How Much Weight Can You Lose?
Weight loss varies by drug, dose, and individual. But the numbers are hard to ignore.
On semaglutide (Wegovy, 2.4 mg weekly), people in clinical trials lost an average of 15.3 kg (about 34 pounds) over 68 weeks. That’s nearly 15% of total body weight. More than half of participants lost 15% or more. In real life, people on Reddit and patient forums report 50, 70, even 100-pound losses over a year or two.
Tirzepatide (Zepbound), a newer dual-action drug that also targets GIP receptors, pushed that even further. In the SURMOUNT-2 trial, users lost an average of 20.9% of their body weight. That’s comparable to what bariatric surgery used to deliver.
Compare that to older diabetes drugs:
- Insulin: Often causes 4-10 kg weight gain
- Sulfonylureas: Typically adds 2-4 kg
- DPP-4 inhibitors: No real weight change
- SGLT2 inhibitors: Lose 2-5 kg-good, but not nearly as much
GLP-1 agonists don’t just outperform other diabetes drugs-they redefine what’s possible.
How Much Does A1C Drop?
A1C measures your average blood sugar over 3 months. Most people with type 2 diabetes start around 8-9%. The goal is under 7%.
Here’s what GLP-1 agonists deliver:
- Semaglutide (Ozempic, 1.0 mg weekly): Drops A1C by 1.8% on average
- Liraglutide (Victoza, 1.8 mg daily): Drops A1C by 1.14%
- Dulaglutide (Trulicity): Around 1.5% reduction
- Tirzepatide (Mounjaro): Up to 2.4% reduction at the highest dose
That’s better than most oral pills. And unlike metformin or sulfonylureas, these drugs lower A1C without causing weight gain-or even while causing weight loss.
Side Effects: What to Expect
These drugs aren’t side effect-free. But most side effects are manageable-and often fade.
The biggest issue? Your stomach. Up to 50% of users feel nausea, especially when starting or increasing the dose. Vomiting affects 5-10%, and diarrhea hits about 25%. These usually peak in the first 4-8 weeks and improve as your body adjusts.
Here’s how to reduce them:
- Start low and go slow. The full dose of Wegovy takes 16-20 weeks to reach.
- Avoid high-fat meals during dose increases-they worsen nausea.
- Take the injection at night. Many people report less nausea when they sleep through the initial wave.
- Use OTC meds like dimenhydrinate (Dramamine) if nausea is strong.
Other side effects are rare: gallbladder issues, pancreatitis, and thyroid tumors (in rodents, not confirmed in humans). The FDA requires a boxed warning for thyroid cancer risk based on animal data, but no human cases have been linked to these drugs so far.
Most people tolerate them well after the first few months. And many say the trade-off is worth it: no more cravings, no more blood sugar spikes, and real weight loss.
Why People Love Them (And Why They’re Hard to Get)
On patient forums, the most common praise isn’t about the scale-it’s about the mental shift.
One user wrote: ‘I no longer crave sugar. It’s like my brain rewired itself.’ Another said: ‘I used to eat just because it was there. Now, I eat because I’m hungry.’
That’s the hidden benefit: these drugs change your relationship with food. You don’t feel deprived. You just don’t want the same things anymore.
But there’s a catch: cost and access.
Without insurance, a month of semaglutide costs $800-$1,200. Even with insurance, many plans require you to try and fail on cheaper drugs first. Medicare Part D covers about 62% of prescriptions-but often only after prior authorization.
And supply? Shortages are real. Since early 2022, semaglutide (Wegovy and Ozempic) has been on the FDA’s shortage list. Doctors report 30% of prescriptions can’t be filled on time. Demand has outpaced production.
What Happens When You Stop?
This is the big question no one talks about enough.
Studies show that if you stop taking GLP-1 agonists, you regain 50-70% of the lost weight within a year. That’s not failure-it’s biology. These drugs aren’t curing obesity. They’re managing it, like blood pressure or cholesterol meds.
That doesn’t make them useless. It just means they’re tools, not cures. Many people plan to use them for 1-2 years to jumpstart weight loss, then transition to lifestyle changes. Others stay on them long-term because their health depends on it.
Experts agree: the goal isn’t to stop. It’s to find the right balance between medication, diet, and movement that works for your life.
How Do They Compare to Newer Drugs?
The field is moving fast. Tirzepatide (Zepbound) is already here, and it’s stronger. It combines GLP-1 with GIP, another gut hormone that boosts insulin and fat burning. In trials, it led to 20.2% weight loss-the highest ever seen in a non-surgical weight drug.
Oral versions are coming. Novo Nordisk has an oral semaglutide pill approved for diabetes (Rybelsus), and they’re testing it for weight loss. If it works as well as the injection, that could change everything-no needles, more access.
Even triple agonists (GLP-1 + GIP + glucagon) are in early trials. Early results suggest even greater weight loss and metabolic benefits.
But for now, semaglutide and tirzepatide are the gold standard. And they’re not just for diabetes anymore.

It’s Not Just About Diabetes
These drugs are being studied for more than weight and blood sugar.
- NAFLD: Semaglutide reduced liver fat by 52% in a 2024 study-better than placebo.
- Heart failure: In the STEP-HFpEF trial, semaglutide improved walking distance and reduced symptoms in obese patients with heart failure.
- Alzheimer’s: Novo Nordisk is testing oral semaglutide to see if it can slow brain decline in early-stage Alzheimer’s.
That’s why doctors now call these drugs ‘metabolic reset’ agents. They’re not just treating one condition-they’re fixing multiple parts of a broken system.
Who Should Consider Them?
You might be a good candidate if:
- You have type 2 diabetes and haven’t reached your A1C goal with other meds
- You have obesity (BMI ≥30) or overweight (BMI ≥27) with a weight-related condition like high blood pressure or sleep apnea
- You’ve tried diet and exercise but keep regaining weight
- You want to reduce your risk of heart disease-these drugs lower cardiovascular events by 13%
You might not be a good fit if:
- You have a personal or family history of medullary thyroid cancer
- You have multiple endocrine neoplasia syndrome type 2
- You can’t commit to weekly injections
- You have severe gastrointestinal disease (like gastroparesis)
Always talk to your doctor. These aren’t over-the-counter supplements. They’re powerful medications that need monitoring.
What’s Next?
GLP-1 receptor agonists are no longer niche. They’re mainstream. In 2023, the global market hit $23.5 billion-and it’s projected to double by 2028. Semaglutide alone made $10.8 billion for Novo Nordisk.
They’ve changed how we treat obesity and diabetes. They’ve made weight loss possible without surgery. They’ve turned a chronic disease into a manageable condition.
But they’re not the end of the story. They’re the beginning of a new era-where medicine doesn’t just treat symptoms, but reprograms metabolism itself.
Do GLP-1 agonists cure diabetes?
No, they don’t cure diabetes. They help manage it by improving blood sugar control, reducing insulin resistance, and lowering A1C. Many people reduce or stop other diabetes medications while on GLP-1 agonists, but most still need to continue the injection to maintain results. Stopping usually leads to a return of higher blood sugar levels.
Can I take GLP-1 agonists if I don’t have diabetes?
Yes. Wegovy and Zepbound are FDA-approved for chronic weight management in adults with obesity (BMI ≥30) or overweight (BMI ≥27) with at least one weight-related condition like high blood pressure, type 2 diabetes, or sleep apnea. You don’t need to have diabetes to qualify for weight loss use.
How long does it take to see weight loss results?
Most people start noticing reduced appetite and slight weight loss within the first 2-4 weeks. Significant weight loss (5% or more of body weight) usually happens by 12-16 weeks. The full effect takes 6-12 months, especially as the dose is gradually increased.
Are GLP-1 agonists safe for long-term use?
Current data shows they’re safe for long-term use. The LEADER trial followed liraglutide users for over 5 years and found no increased risk of serious side effects. In fact, they reduced heart attacks, strokes, and heart-related deaths in high-risk patients. Long-term safety for newer drugs like tirzepatide is still being studied, but early results are promising.
Why are these drugs so expensive?
Manufacturing these complex biologic drugs is costly. Demand has exploded, outpacing supply. Companies like Novo Nordisk and Eli Lilly are investing heavily in production, but it takes years to scale. Insurance coverage varies widely, and without it, out-of-pocket costs can be $1,000/month. Some manufacturers offer savings cards, but they don’t cover everyone.
Do I need to change my diet while taking GLP-1 agonists?
You don’t have to follow a strict diet, but eating balanced meals helps. These drugs reduce cravings, so junk food becomes less appealing. But eating too many high-fat or sugary foods can still cause nausea or slow progress. Many users naturally eat less and choose healthier options without forcing themselves.


