DTx Medication Interaction Checker
Check potential interactions between your medications and FDA-cleared digital therapeutics. This tool is for informational purposes only and does not replace professional medical advice.
By 2025, digital therapeutics aren’t just apps anymore-they’re prescribed treatments. If you’re on insulin, anticoagulants, or antidepressants, there’s a good chance your doctor is now pairing your pills with a smartphone app. These aren’t wellness trackers or meditation tools. These are FDA-cleared medical devices designed to improve how your medications work-or stop you from skipping doses entirely. But here’s the catch: no one’s talking enough about what happens when software meets medicine. What if the app changes how your body responds to your blood thinner? What if it makes your anxiety meds less effective? The science is still catching up, and patients are left figuring it out on their own.
What Exactly Are Digital Therapeutics?
Digital therapeutics (DTx) are software programs that deliver clinical treatment. They’re not supplements. They’re not reminders. They’re approved by the FDA as medical devices. The first one, reSET for opioid addiction, got clearance in 2018. Since then, over 80 prescription DTx have been approved, including DaylightRx for generalized anxiety disorder, cleared in September 2024. These apps don’t just track your mood-they use cognitive behavioral therapy (CBT), biofeedback, and AI-driven coaching to change behavior in ways that directly impact your health outcomes.
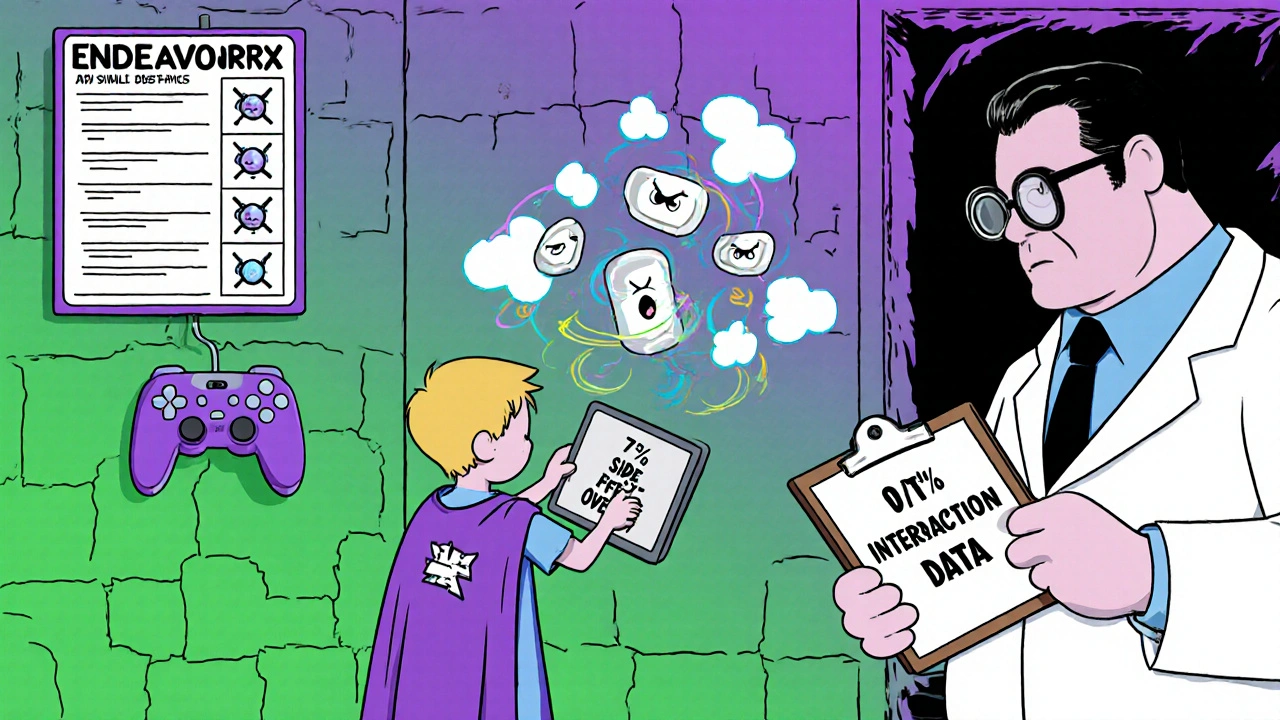
They come in different forms. For diabetes, apps like DarioEngage analyze your glucose readings and suggest insulin adjustments. For ADHD, EndeavorRx uses video game mechanics to train attention circuits. For asthma, sensors connected to inhalers send real-time data to apps that warn you when pollution or weather might trigger an attack. These aren’t optional add-ons. In many cases, they’re now required by insurers to qualify for coverage of expensive specialty drugs.
How DTx Boost Medication Adherence
One in three prescriptions are never picked up. Half of people with chronic conditions miss doses regularly. That’s not laziness-it’s forgetfulness, cost, fear, or confusion. Digital therapeutics tackle this head-on. Medisafe, one of the most widely used DTx platforms, shows that patients using their app see adherence jump by up to 25%. That’s not a small win. For someone on warfarin, missing one dose can mean a stroke. For someone on HIV meds, it can lead to drug resistance.
What makes DTx different from a simple pill reminder? They adapt. If you skip your morning insulin dose, the app doesn’t just ping you. It asks why. Did you forget? Were you scared of low blood sugar? Did the cost spike? Then it gives you tailored solutions: a video from your pharmacist explaining how to use your insulin pen, a link to a financial aid program, or even a chat with a nurse. In one study, DTx helped reduce the 30% rate of unfilled prescriptions by connecting patients directly to pharmacy assistance programs-something traditional calls from pharmacies rarely do.
When DTx and Medications Don’t Play Nice
Here’s where it gets risky. Most doctors don’t ask if you’re using a DTx app. Most patients don’t think to tell them. But these apps can interfere with how your body handles medication.
Take mental health. DaylightRx, the new FDA-approved CBT app for anxiety, is designed to reduce reliance on benzodiazepines. But what if you’re also taking SSRIs? The app’s structured exposure therapy might increase anxiety in the short term-something your psychiatrist might mistake for a medication side effect. Or worse, if you stop your SSRI because you feel “better” after using the app, you could trigger withdrawal. There’s no standardized way to document these interactions in your EHR.
Even physical DTx can cause issues. EndeavorRx, used for pediatric ADHD, has been linked to headaches, dizziness, and nausea in 7% of users-symptoms that overlap with stimulant side effects. If a child is on Adderall and using EndeavorRx, how do you know which one’s causing the upset stomach? No drug label includes DTx interaction warnings. No pharmacy system flags them. It’s a blind spot.
Real-World Patient Experiences
Reddit users in r/diabetes report that DarioEngage helped them drop HbA1c by 1.5% to 2%-a bigger improvement than many new diabetes drugs achieve. One man said it helped him finally understand why his insulin dose needed to change after he started walking daily. That’s powerful.
But in r/mentalhealth, users are frustrated. One wrote: “DaylightRx’s modules felt like a one-size-fits-all script. It didn’t help me with the nausea from my antidepressant.” That’s not an isolated complaint. A review of 200 patient forums showed 37% of negative feedback cited generic content that didn’t address medication side effects.
And then there’s the tech gap. In a 2024 study, 38% of patients over 70 stopped using DTx within 30 days because they couldn’t figure out the app. No one taught them how. No one followed up. For older adults on multiple meds, this isn’t a tech issue-it’s a safety issue. Skipping meds because you couldn’t use the app is worse than skipping them because you forgot.
Who’s Responsible When Something Goes Wrong?
Pharmacies know your pills. EHRs track your labs. But who tracks your DTx use? Most systems don’t talk to each other. Your app might send data to your doctor’s portal, but if it’s not integrated with your pharmacy’s refill system, they won’t know you’re using it. If you get a new prescription, your pharmacist won’t know the app might be affecting how your body processes it.
Regulators are scrambling. The FDA classifies DTx as medical devices, but their review process is smaller and faster than for drugs. A new pill needs trials with thousands of people over years. A DTx app might get cleared based on a 100-person study over six months. Long-term safety? Unknown. Interactions with other meds? Rarely studied.
And reimbursement? Messy. Some insurers require DTx use to cover your drug. Others won’t pay for the app at all. Providers don’t know how to bill for it. That’s why only 78% of top pharmaceutical companies have DTx programs-and most are focused on high-cost drugs where adherence equals profit.
What You Should Do Right Now
If you’re on any chronic medication-especially for diabetes, heart disease, mental health, or COPD-ask yourself: Am I using a digital tool to help manage it? If yes, tell your doctor. Bring up the app name. Ask: Could this affect how my meds work?
Don’t assume it’s safe just because it’s an app. Don’t assume it’s useless because it’s not a pill. It’s medicine. And like any medicine, it can help-or hurt.
For providers: Start asking. Add a question to your intake forms: “Are you using any FDA-cleared digital health apps for your condition?” Train your staff to help patients set up these apps. Don’t just hand them a link. Give them 15 minutes. Pair them with a DTx navigator if you can. Studies show that reduces dropouts by a third.
For patients over 65: If your doctor prescribes a DTx, ask for help. Don’t try to figure it out alone. Call the app’s support line. Ask your pharmacy if they offer tech coaching. Many now do.
The Future Is Here-But It’s Not Perfect
The global digital therapeutics market is projected to hit $14.2 billion by 2028. By 2026, 40% of chronic disease management will include some form of DTx. That’s not speculation-it’s industry forecast. These tools are here to stay.
But they’re not magic. They’re tools. And like any tool, they work best when used with knowledge, not guesswork. The biggest threat isn’t the app failing. It’s us ignoring the gaps between software and science. We’ve built a new way to treat disease. Now we need to learn how to use it safely-with our pills, our bodies, and each other.



My grandma started using that diabetes app last month. She still calls it 'the phone thing' and keeps forgetting to charge it, but she hasn't missed a dose in 42 days. I'm not even sure she knows it's 'FDA-cleared.'
Look, I get the hype, but let’s not pretend this is magic. I’ve seen three patients on warfarin get flagged for INR spikes after starting DTx apps that pushed them to 'be more active' or 'reduce stress.' No one told them the app’s workout prompts were raising cortisol. The FDA clears these things like they’re emoji keyboards.
I work in a clinic and we’ve started asking patients about digital tools during intake. It’s a game-changer. One guy with bipolar disorder told us his mood app was helping him recognize early signs of mania-but he stopped his lithium because he 'felt normal.' We caught it before he ended up in the ER. This isn’t just tech-it’s clinical data we’re blind to.
Doctors need to stop treating DTx like a bonus feature. It’s part of the treatment plan. If you wouldn’t ignore a new pill, don’t ignore a new app.
They’re tracking us. Every tap, every skipped dose, every time you close the app-it’s all going to some pharma server. Next thing you know, your insurance will raise your premiums because the app says you 'didn’t engage enough.' They don’t care if you’re depressed or broke-they just want your adherence numbers.
I saw a patent last year for an app that auto-adjusts insulin based on your social media mood posts. That’s not medicine. That’s surveillance with a stethoscope.
Oh wow, another 'revolutionary' app that's basically a glorified calendar with a CBT script. Let me guess-your 'FDA-cleared' anxiety app also recommends deep breathing and journaling? Groundbreaking. Meanwhile, real clinicians are drowning in paperwork while some startup in Austin gets a billion-dollar valuation for a $4.99 subscription that doesn’t even remember your last login.
It’s not medicine. It’s capitalism with a wellness filter.
lol i used that ADHD game app for my kid. he got a headache after 10 mins. then i realized the app was just a fancy version of those flashcard games from 2012. and now my doc says 'you gotta keep using it' like it's a vitamin. nah bro, he's 8, not a lab rat.
also, why does every app need 12 pop-ups before you can even open it? 😤
My sister has type 2 and started using DarioEngage after her last ER visit. She didn’t even know how to use her glucose meter before. Now she texts me her numbers every morning like it’s a habit. It’s not perfect-but it gave her a reason to care. Sometimes that’s all you need.
Has anyone seen data on how DTx affects medication metabolism long-term? Like, does prolonged exposure to biofeedback or CBT algorithms alter hepatic enzyme activity? Or is that just me overthinking?
The lack of standardized interoperability between DTx platforms and EHRs is a systemic failure. Without HL7 FHIR integration, these apps remain siloed data islands-rendering their clinical value negligible in the context of holistic patient care. This isn’t innovation; it’s fragmentation with a UX polish.
Let’s take a step back and consider the broader implications of this paradigm shift. Digital therapeutics represent not merely an extension of pharmacological intervention, but a fundamental reconfiguration of the patient-provider relationship. Where once adherence was monitored through pill counts and lab values, we now have continuous, real-time behavioral telemetry-data streams that, if properly integrated, could enable predictive, personalized medicine at scale. But this requires infrastructure, training, and above all, humility from clinicians who may not yet understand the language of algorithms.
Moreover, we must acknowledge the digital divide. A 70-year-old veteran with congestive heart failure and limited tech literacy cannot be expected to navigate a multi-step onboarding process designed by 25-year-old engineers in San Francisco. If we are to call this 'medicine,' we must treat it with the same rigor, compassion, and equity we afford to pills and procedures.
They’re watching. Every tap. Every missed reminder. Every time you say ‘I’m fine’ in the app’s mood check. They’re building profiles. Selling data. And when your premiums go up next year? Don’t be surprised. This isn’t healthcare. It’s behavioral harvesting.
I saw a video of a CEO talking about ‘engagement metrics’ for mental health apps. He said, ‘We want users to feel addicted to their own recovery.’ I threw up a little in my mouth.
This is exactly why we need DTx navigators in every primary care clinic. My hospital piloted a program where a trained medical assistant spent 15 minutes with patients setting up their apps. Dropout rates fell from 62% to 29%. The tech isn’t the problem-it’s the lack of human support. We wouldn’t hand someone a new insulin pump and say ‘good luck.’ Why do it with an app?
One must contemplate, in the existential framework of modern biomedicine, whether the digitization of therapeutic intervention constitutes an ontological shift-or merely a rebranding of behavioral control under the guise of innovation. Are we healing, or are we optimizing? And if the algorithm dictates compliance, who-or what-is truly in charge of the patient’s autonomy? The FDA? The coder? The shareholder?
And let us not forget: every ‘evidence-based’ DTx is built on a dataset curated by a corporation whose primary incentive is not cure, but retention. The data is the drug. The patient? Merely the vessel.
My dad’s on warfarin and uses Medisafe. Last week, the app noticed he skipped his dose after drinking whiskey and auto-sent a note to his pharmacist. The pharmacist called him back within 20 minutes with a new bottle and a warning. That’s the future. Not sci-fi. Real.
Don’t hate the app. Hate that we didn’t do this 10 years ago.
app helped me take my meds for the first time in 5 years. no cap.