Imagine taking a statin to lower your cholesterol, then adding an antibiotic for a sinus infection - and within days, your muscles start aching, your urine turns dark, and you feel like you’ve been hit by a truck. This isn’t rare. It’s rhabdomyolysis, a dangerous condition where muscle tissue breaks down and floods your bloodstream with toxic debris. And more than half the time, it’s not from overtraining or trauma - it’s from two perfectly legal medications interacting in your body.
What Exactly Is Rhabdomyolysis?
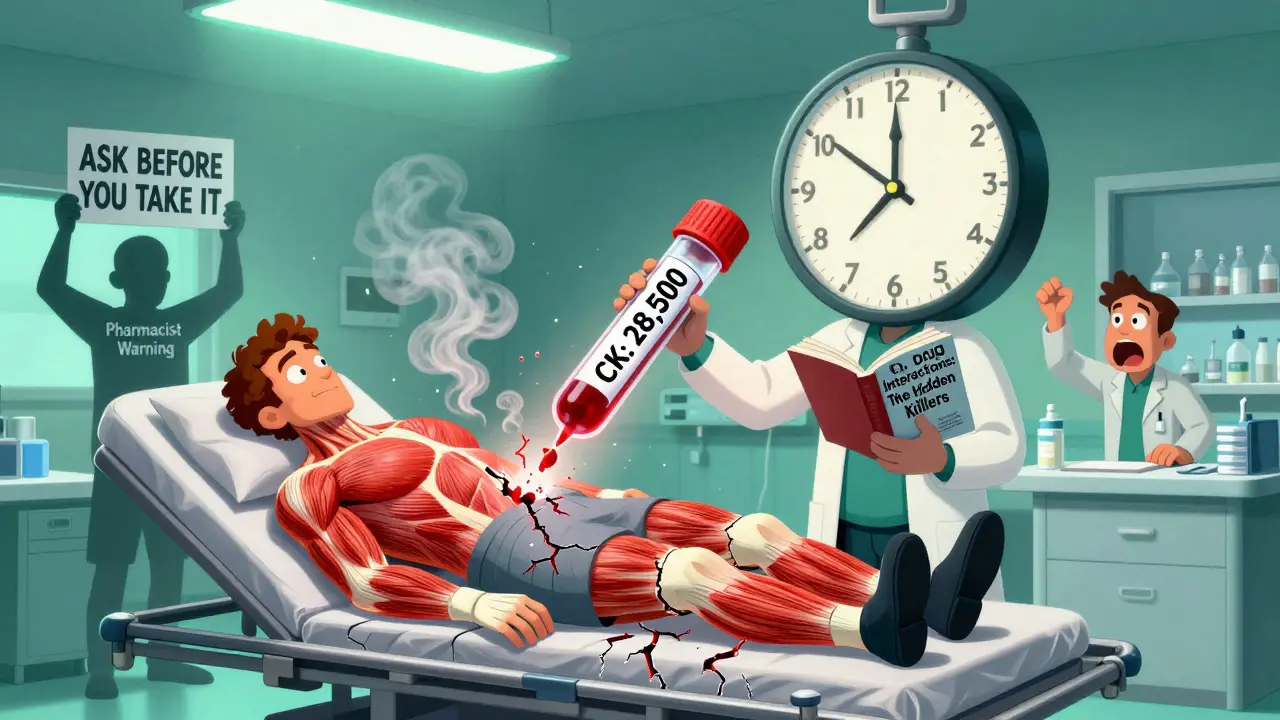
Rhabdomyolysis happens when muscle cells rupture and spill their contents - especially creatine kinase (CK), potassium, and myoglobin - into your blood. Myoglobin is the real danger. Your kidneys try to filter it out, but it clogs the tiny tubes inside them, leading to acute kidney injury. In severe cases, you’ll need dialysis. About 50% of people with drug-induced rhabdomyolysis develop kidney damage. Around 1 in 10 don’t survive.The classic signs - muscle pain, weakness, and dark urine - show up in only about half the cases. Many people just feel tired, nauseous, or have abdominal pain. Some don’t notice anything until they’re in the ER with no urine output. That’s why it’s so often missed.
Which Medications Are the Biggest Culprits?
Statins are the number one cause. About 60% of all medication-related rhabdomyolysis cases come from these cholesterol-lowering drugs. Atorvastatin (Lipitor) and simvastatin (Zocor) make up nearly 80% of those cases. But here’s the catch: statins alone are usually safe. The real risk comes when they’re combined with other drugs.Take gemfibrozil, a fibrate used for triglycerides. When paired with simvastatin, the risk of rhabdomyolysis jumps 15 to 20 times. Why? Both drugs are processed by the same liver enzyme - CYP3A4. When one blocks it, the other builds up to toxic levels. It’s like pouring gasoline on a fire.
Antibiotics like erythromycin and clarithromycin are equally dangerous. A 2020 study found that combining clarithromycin with colchicine - a common gout treatment - caused rhabdomyolysis in 8.7% of patients. One Reddit user described it perfectly: “Added clarithromycin to my colchicine for gout. My urine turned cola-colored in 48 hours. CK hit 28,500.”
Even cancer drugs can trigger it. Erlotinib, used for lung cancer, combined with simvastatin, has been linked to CK levels over 20,000 U/L in under 72 hours. And propofol, the anesthesia drug used in ICUs, causes a rare but deadly form called propofol infusion syndrome. When it leads to rhabdomyolysis, mortality hits 68%.
Who’s Most at Risk?
It’s not random. Certain people are far more vulnerable.- People over 65 - their risk is 3.2 times higher.
- Women - they’re 1.7 times more likely than men to develop it.
- Those with kidney problems - if your eGFR is below 60, your risk spikes 4.5 times.
- Anyone taking five or more medications - that group has a 17.3 times higher risk.
There’s also a genetic factor. About 1 in 5 people of European descent carry the SLCO1B1*5 gene variant. It makes them 4.5 times more likely to get muscle damage from simvastatin. Most doctors don’t test for it - but if you’ve had unexplained muscle pain on statins before, you might have it.
How Do These Interactions Actually Happen?
It’s all about how your body breaks down drugs. The liver uses enzymes - mainly CYP3A4 - to metabolize most medications. When two drugs compete for the same enzyme, one can block it. That causes the other to build up to dangerous levels.For example:
- Simvastatin + clarithromycin = 18.7x higher risk
- Simvastatin + itraconazole (antifungal) = 12x higher risk
- Colchicine + verapamil (blood pressure drug) = 14.2x higher risk
Even over-the-counter supplements can be risky. St. John’s Wort, often used for mild depression, can interfere with statin metabolism. Grapefruit juice? It’s a known CYP3A4 inhibitor. One glass a day can raise simvastatin levels by 300%.
What Happens When You Go to the Hospital?
If you’re admitted with suspected rhabdomyolysis, here’s what happens:- Your CK level is checked. Anything above 1,000 U/L is abnormal. Severe cases hit 5,000 to over 100,000.
- You get IV fluids - usually 3 liters in the first 6 hours, then 1.5 liters per hour. The goal? Flush out myoglobin before it kills your kidneys.
- Sodium bicarbonate is added to keep your urine pH above 6.5. This prevents myoglobin from clumping in your tubules.
- Your potassium, calcium, and kidney function are monitored hourly. High potassium can stop your heart. Low calcium can cause seizures.
- The offending drug is stopped - immediately.
Some cases need plasma exchange, especially if the drug has a long half-life. Leflunomide, used for rheumatoid arthritis, sticks around for two weeks. Without plasma exchange, it keeps damaging muscle cells.
Recovery - It’s Not Just About Surviving
Surviving doesn’t mean going back to normal. A 10-year Mayo Clinic study found that 43.7% of survivors still had muscle weakness six months later. Full recovery takes 12 to 28 weeks, depending on whether you needed dialysis.And the damage doesn’t always show up on blood tests. Many people report ongoing fatigue, stiffness, and reduced strength - even after their CK levels return to normal. That’s why follow-up with a physical therapist matters.

Why Are Doctors Missing This?
A 2022 survey of 147 statin-induced rhabdomyolysis cases on Reddit found that 92% of patients said their doctor never warned them about the risks of combining medications. Many doctors assume statins are safe because they’re prescribed so often. But the data doesn’t lie: 89% of fatal cases involve drug interactions - even though those combinations make up only 12% of all statin prescriptions.The FDA and EMA have issued warnings. In 2021, the EMA forced all colchicine labels to include strong CYP3A4 inhibitor warnings. In 2023, statin labels now must list exact contraindications. But warnings on a label don’t change practice if doctors don’t ask about all medications - including supplements and OTC drugs.
How to Protect Yourself
You can’t control everything - but you can control this:- Know your meds. Keep a written list of everything you take - prescriptions, supplements, even herbal teas.
- Ask your pharmacist. Pharmacists are trained to spot dangerous interactions. Ask: “Could any of these cause muscle damage?”
- Speak up about muscle pain. If you feel new, unexplained soreness - especially after starting a new drug - don’t wait. Get a CK test.
- Avoid grapefruit. If you’re on a statin, skip it. Even one glass can be risky.
- Get tested if you’re over 65 or on 5+ drugs. Your risk isn’t theoretical. It’s mathematical.
There’s no magic bullet. But catching rhabdomyolysis early can mean the difference between a week in the hospital and a lifetime on dialysis.
What’s Being Done to Stop This?
The NIH is funding a $2.4 million project to build a real-time drug interaction alert system that flags high-risk combinations before they’re prescribed. The European Renal Association is testing new drugs that protect mitochondria from statin damage. And hospitals are starting to screen high-risk patients for the SLCO1B1 gene.But until those systems are everywhere, you’re your own best defense. If you’re on statins and your doctor adds a new medication - whether it’s an antibiotic, antifungal, or even a sleep aid - ask: “Could this cause muscle breakdown?”
It’s not paranoia. It’s survival.
Can rhabdomyolysis happen from just one medication?
Yes, but it’s rare. Most cases (over 80%) involve drug interactions. Statins alone can cause it, especially at high doses or in older adults with kidney issues. But combining them with other drugs - like antibiotics, antifungals, or fibrates - increases the risk dramatically, often by 10 to 20 times.
How do I know if my muscle pain is serious?
Normal soreness from exercise fades in a day or two. If your pain is deep, persistent, and not tied to activity - especially if you’ve recently started a new medication - it could be serious. Watch for dark, tea- or cola-colored urine. That’s a red flag. Don’t wait. Get a creatine kinase (CK) blood test.
Are all statins equally risky?
No. Simvastatin and lovastatin are the riskiest because they’re heavily processed by the CYP3A4 enzyme. Atorvastatin carries moderate risk. Pravastatin and rosuvastatin are much safer - they’re cleared differently and rarely cause rhabdomyolysis, even with interacting drugs. If you’re on a high-risk statin and need a new medication, ask if switching is an option.
Can I take statins if I have kidney disease?
You can - but with caution. If your eGFR is below 60, your risk of rhabdomyolysis jumps 4.5 times. Your doctor should lower your statin dose or switch you to a safer option like pravastatin or rosuvastatin. Never stop statins without talking to your doctor - the heart benefits often outweigh the risks. But you need close monitoring.
Is there a blood test to confirm rhabdomyolysis?
Yes. The creatine kinase (CK) test is the gold standard. A level above 1,000 U/L is diagnostic. In severe cases, it can exceed 100,000 U/L. Other signs include elevated potassium, low calcium, and myoglobin in urine. But CK is the most reliable. If you’re on multiple medications and have unexplained muscle pain, ask for this test - don’t wait for symptoms to worsen.


So let me get this straight - we’re giving people statins like they’re candy, then slapping on antibiotics like it’s a flavor topping, and acting shocked when their muscles turn into soup? 🤦♀️ I’ve seen this in my ER rotation. One guy took Lipitor + clarithromycin for a sinus thing. Came in with urine the color of a bourbon neat. CK was higher than my student loan balance. He didn’t even know grapefruit juice was a thing. We’re not treating patients. We’re playing Russian roulette with a pharmacy.
And nobody talks about the genetic angle. SLCO1B1*5? Most docs don’t even know what that is. Meanwhile, grandma’s on five meds, drinks grapefruit juice every morning, and thinks ‘muscle soreness’ is just getting old. It’s not aging. It’s pharmacology negligence.
Why do we wait for someone to need dialysis before we ask, ‘Wait - what else are you taking?’
statins r the worst. i got muscle pain after 3 days. doc said ‘it’s just soreness’ - yeah right. CK was 14k. they put me on iv fluids like i was a dehydrated camel. now i’m scared to take anything. even tylenol makes me nervous. #rhabdoawareness
One cannot help but observe the alarming epistemological collapse within contemporary pharmacovigilance - wherein the clinical judgment of the physician is subordinated to the commodified logic of pharmaceutical marketing, and the patient, reduced to a mere data point, is left to navigate a labyrinth of enzyme kinetics and metabolic pathways they were never taught to understand.
Moreover, the casual dismissal of ‘muscle soreness’ as benign is not merely negligent - it is a metaphysical betrayal of the Hippocratic Oath’s foundational tenet: Primum non nocere. And yet, here we are - 2025 - still waiting for the system to catch up to the science.
It is not paranoia. It is precision.
Thank you for sharing this. I’m so glad someone’s talking about it. I was scared to say anything when my legs felt heavy after starting a new antibiotic - but I got my CK checked. Thank you for giving me the courage to ask. You’re right - it’s not just ‘getting older.’
While I appreciate the comprehensive nature of this post, I would like to respectfully suggest that the emphasis on genetic predisposition, while scientifically valid, may inadvertently contribute to patient anxiety without sufficient access to affordable genetic screening. A more equitable public health approach would prioritize pharmacist-led medication reconciliation and standardized electronic health record alerts - rather than placing the burden of metabolic literacy on the individual.
Also, typo: ‘eGFR is below 60’ - should be ‘eGFR < 60 mL/min/1.73m²’ for clinical precision.
This is exactly the kind of information that needs to be in every primary care waiting room. I’ve had patients come in with CK levels over 50,000 and no idea why. They were on simvastatin + diltiazem for blood pressure, and their pharmacist never flagged it. I’m going to print this out and put it on the bulletin board tomorrow.
Also - if you’re on statins and you’re over 65, please, please ask your doctor about pravastatin or rosuvastatin. The difference in risk is real.
And yes - grapefruit juice is not your friend.
Wait - so my uncle who died after a ‘routine’ antibiotic prescription… was it this? He was on Lipitor. Took azithromycin. Said his legs felt like concrete. Then he couldn’t pee. They said ‘kidney failure.’ But no one said why.
I’m gonna scream now. I’m gonna tell every family member I have. This isn’t rare. It’s silent. And it’s happening to people we love.
Why aren’t pharmacists screaming this from the rooftops? Why do we have to Google ‘dark urine after antibiotics’ to find out we might be dying?
Wow. Another fear-mongering anti-pharma rant disguised as medical advice. Statins save millions. The risk of rhabdomyolysis is 1 in 10,000. You’re scaring people into stopping life-saving meds because of a handful of anecdotal Reddit posts. The real problem? People don’t follow instructions. Take your statin. Don’t drink grapefruit juice. Done.
Also - CK 28,500? That’s not a ‘Reddit user’ - that’s a case study. You’re conflating outliers with epidemiology. Pathetic.
omg yes!! i had this happen to me 😭 i took zocor + cipro and my legs felt like jelly. i thought i was just tired. then my pee turned brown. i called my mom crying. she made me go to er. they said ‘you’re lucky you came in when you did.’ now i keep a meds list on my phone. and i never touch grapefruit. 🍊❌
AMERICA IS BEING POISONED BY BIG PHARMA AND THEIR LAZY DOCTORS. THEY DON’T CARE ABOUT YOU. THEY WANT YOU ON DRUGS FOREVER. THIS ISN’T MEDICINE - IT’S CORPORATE MASS MURDER. IF YOU’RE ON STATINS, YOU’RE ONE PRESCRIPTION AWAY FROM A KIDNEY TRANSPLANT. STOP TRUSTING THEM. STOP TAKING THEM. YOUR BODY ISN’T A LAB RAT.
Everyone’s missing the real issue: the FDA’s approval process is broken. They approved simvastatin in 1996 without proper interaction studies. The CYP3A4 conflict was known since the 80s. This isn’t ‘rare’ - it’s institutionalized malpractice. And now we’re supposed to be grateful for a label update in 2023? Pathetic. The system is designed to fail you - and you’re still taking the pills.
I work in a community pharmacy and see this every week. A patient comes in with a new script for clarithromycin - same day they’re picking up simvastatin. We flag it. Sometimes they say ‘my doctor said it’s fine.’ We call the doctor. Sometimes they say ‘I forgot to check interactions.’
We’re the last line of defense. And we’re overworked.
Don’t assume your doctor knows every interaction. Ask us. We’re here to help.
Also - if you’re on colchicine and have gout, please, please ask about alternatives. The risk with macrolides is terrifying.
Let’s be real - if you’re over 60, on more than three meds, and you’ve ever had a muscle cramp after starting something new… you’ve already had a near-miss. You just didn’t know it.
And yes - I’ve seen the ‘I feel fine’ crowd. They’re the ones who end up in the ICU. Not because they’re dumb. Because no one told them. The system doesn’t warn you - it punishes you.
And yes - I’ve told my mom to stop taking that herbal tea. ‘It’s just chamomile.’ Yeah. And chamomile inhibits CYP3A4. So does turmeric. So does black pepper. You’re not ‘natural.’ You’re a walking pharmacokinetic storm.
Hey - if you’re reading this and you’re on statins? You’re not alone. I was too scared to ask my doctor about muscle pain. But I did. Turns out I had a mild CK elevation - nothing dangerous, but it made me aware.
Don’t wait for dark urine. Don’t wait for dialysis. Just ask: ‘Could this hurt my muscles?’
It’s not weakness. It’s wisdom.
And if you’re a doctor reading this? Thank you. You’re doing important work. Keep asking the hard questions.
💙
bro i took lipitor + clarithromycin for a cold. 2 days later i couldnt lift my arm. thought i had a heart attack. went to er. they were like ‘oh yeah that’s a thing.’ i was like ‘wait… this is a thing??’
now i have a meds list on my fridge. and i tell every friend i know. you’re not being paranoid. you’re being smart.
also grapefruit is evil. 🍊💀
Chris Van Horn - you’re right. Statins save lives. But they don’t save lives if you’re dead from kidney failure because your doctor didn’t check your meds.
1 in 10,000? That’s 100 people in the US alone every year. And most of them? They didn’t know they were at risk.
It’s not fear-mongering. It’s harm reduction.
And the fact that you think ‘just don’t drink grapefruit juice’ is a solution… that’s the problem.
We need systems. Not slogans.