Getting a filling, a cleaning, or even having a tooth pulled shouldn’t be scary - but if you’re on blood thinners, it’s easy to worry. You’ve probably heard stories about people stopping their medication before dental work. That used to be standard advice. But today, blood thinners are managed very differently - and for good reason.
Why You Shouldn’t Stop Your Blood Thinners (Usually)
Most people on anticoagulants don’t need to stop them for dental work. In fact, stopping them can be more dangerous than keeping them. The real risk isn’t bleeding - it’s a clot. A clot can cause a stroke, heart attack, or pulmonary embolism. Studies show that stopping even one blood thinner for a simple dental procedure raises your chance of a serious clot by up to 30%. Meanwhile, the risk of serious bleeding from a filling or extraction is less than 1%. That’s not a fair trade. The American Dental Association, Stanford Health Care, and the Scottish Dental Clinical Effectiveness Programme all agree: don’t stop your medication unless your doctor says otherwise. This isn’t a new idea - it’s been the standard since 2013, and updated again in 2022 and 2023. Dentists now know how to handle bleeding safely without touching your meds.Types of Blood Thinners - And How They Affect Your Dental Visit
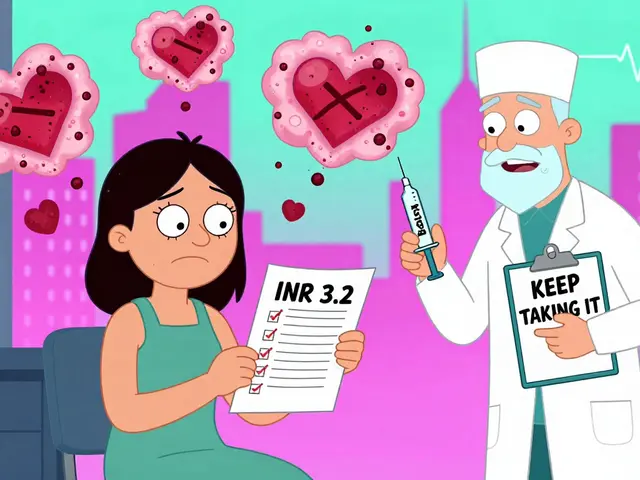
Not all blood thinners are the same. There are two main types: warfarin (a VKA) and DOACs (direct oral anticoagulants). Each has different rules. Warfarin (like Coumadin) requires regular blood tests to check your INR level. This number tells your doctor how long your blood takes to clot. For most dental work:- INR under 3.5? You’re fine for cleanings, fillings, root canals, and even single extractions.
- INR above 3.5? Your dentist will check with your doctor before proceeding.
What Dental Procedures Are Safe? (Bleeding Risk Categories)
Not all dental work is equal. Here’s how experts break it down:- Low risk: Routine cleanings, X-rays, impressions, simple exams. No changes needed.
- Low-moderate risk: Fillings, root canals, scaling and planing (deep cleaning). No changes needed.
- Moderate risk: One to three simple extractions, gum surgery, crown prep. Usually no changes. If INR is high, local hemostatic measures are used.
- High risk: Multiple extractions, complex oral surgery, bone grafts. May require holding warfarin 3-5 days or skipping one DOAC dose. Always coordinated with your doctor.

What Your Dentist Will Do to Control Bleeding
If you’re on blood thinners, your dentist isn’t just going to pull the tooth and hope for the best. They’re trained to stop bleeding fast - and they have tools for it.- Tranexamic acid mouthwash: A special rinse (5% solution) you hold in your mouth for 1-2 minutes after the procedure. It helps clots form. You can use it every 2 hours for up to 24 hours. It’s safe, effective, and doesn’t interfere with your meds.
- Pressure and sutures: Gauze, dissolvable stitches, or even a special dental gel can seal the area.
- Avoiding multiple extractions: If you need more than two teeth out, your dentist will space them out over two visits. Less trauma. Less bleeding.
- No NSAIDs: They’ll avoid prescribing ibuprofen or aspirin. Even a single tablet can increase bleeding risk.
What You Should Do Before Your Appointment
You’re not just a patient. You’re part of the team. Here’s how to help:- Bring your medication list: Write down every drug - even over-the-counter ones. Include dosages and when you take them.
- Know your INR if you’re on warfarin: If your last test was more than a week ago, ask your doctor for a recent result. Bring it with you.
- Don’t stop your meds: Not even for one day. Not unless your doctor says so in writing.
- Ask questions: If your dentist says you need to stop your blood thinner, ask why. Ask for the guideline they’re following. Most will be happy to consult your doctor.
What to Watch For After Your Procedure
Some oozing is normal. Swirling pink saliva? That’s fine. Bright red blood soaking through gauze? That’s not.- Normal: Light pink for a few hours. Slight discomfort.
- Call your dentist if: Bleeding doesn’t slow after 2 hours of pressure. You’re swallowing blood. You feel dizzy or weak. The clot falls out and the socket starts throbbing.

Common Myths - Debunked
- Myth: You need to stop blood thinners before any dental work. Truth: Only high-risk procedures might need a short hold - and only with your doctor’s approval.
- Myth: Blood thinners always cause dangerous bleeding. Truth: Less than 5% of patients on warfarin have any bleeding complication during dental work - and most are minor.
- Myth: Dentists don’t know how to handle this. Truth: 78% of U.S. dental practices now follow ADA guidelines for anticoagulated patients. They’re trained.
- Myth: If you’re young and healthy, you don’t need blood thinners. Truth: We’re seeing more young patients - athletes with AFib, postpartum women with clots, even 25-year-olds after a blood clot from a flight. Age doesn’t protect you.
When You Need to Talk to Your Doctor
Your dentist doesn’t make the final call on your meds. They coordinate with your doctor. You should talk to your doctor if:- Your INR is above 3.5 (for warfarin users).
- You’re on multiple anticoagulants or antiplatelets (like aspirin + clopidogrel).
- You have kidney or liver disease - it changes how your body processes these drugs.
- You’re pregnant or breastfeeding.
- You’ve had a clot in the last 3 months.
The Bottom Line
You can get your teeth cleaned. You can get fillings. You can even get teeth pulled - safely - while on blood thinners. The key isn’t stopping your medication. It’s communication. Tell your dentist what you’re taking. Bring your latest lab results. Follow their instructions. And don’t let fear keep you from care. The risks of skipping dental work - infection, pain, tooth loss - are far greater than the risks of bleeding. The science is clear. The guidelines are solid. And dentists today are better equipped than ever to keep you safe - without interrupting your life.Can I keep taking my blood thinner before a tooth extraction?
Yes, for most single extractions. You don’t need to stop warfarin or DOACs unless you’re having multiple extractions or major surgery. Even then, it’s often just skipping one dose of a DOAC, not stopping the drug entirely. Always check with your dentist and doctor first.
What if my INR is too high for a dental procedure?
If your INR is above 3.5 (for low-risk procedures) or above 3 (for moderate ones), your dentist won’t proceed without consulting your doctor. They may ask for a quick INR test or recommend holding warfarin for 1-3 days. Never adjust your dose yourself - this must be done under medical supervision.
Do I need to stop aspirin before dental work?
Usually not. If you’re on low-dose aspirin for heart protection, it’s safer to keep taking it. Stopping it increases your risk of a heart attack or stroke more than it reduces bleeding risk. Your dentist will use local measures to control bleeding instead.
Can I use ibuprofen after a dental procedure if I’m on blood thinners?
No. Ibuprofen, naproxen, and other NSAIDs increase bleeding risk when combined with anticoagulants. Your dentist will recommend acetaminophen (paracetamol) instead for pain relief. Always check before taking any OTC painkiller.
How long should I use the tranexamic acid mouthwash?
Use it every 2 hours for the first 24 hours after your procedure. Swish 10mL in your mouth for 1-2 minutes, then spit - don’t swallow. The solution lasts 5 days if refrigerated. It’s safe, effective, and doesn’t interact with your blood thinners.
Are DOACs safer than warfarin for dental procedures?
They’re easier to manage. DOACs don’t require regular blood tests, and they have fewer food and drug interactions. For most dental work, you just skip your morning dose if needed. Warfarin requires INR monitoring and more careful timing. But both are safe when managed correctly.


so like... i just stopped my eliquis before my last cleaning bc my cousin said her dentist made her do it? turns out i was lucky i didn't stroke. thanks for this. i'm gonna print this out and tape it to my fridge. 🙏
It's fascinating how medical dogma shifts so slowly despite overwhelming evidence. For decades, we were told to halt anticoagulants preemptively - a reflexive safety measure born of fear, not data. Now we know the real danger isn't bleeding - it's thrombosis. The statistical asymmetry is staggering: 30% increased clot risk versus under 1% serious hemorrhage. This isn't just a clinical update - it's a philosophical pivot in how we weigh risk. We've been conditioned to avoid bleeding like the plague, but we've ignored the silent, deadlier threat. The real innovation isn't in the drugs - it's in the mindset.
my dentist just asked me what i was on and wrote it down. no big deal. i brought my pill bottle and he nodded like it was normal. honestly? i was expecting a whole drama. turns out they've got this figured out. just tell 'em what you're on and don't panic. tranexamic rinse? yeah, i used it. tasted like soap but worked. no bleeding after my extraction. chill.
One must question the institutionalization of medical protocols. The ADA's endorsement is not infallible. Pharmaceutical influence is pervasive. Are we certain that DOACs, with their lack of routine monitoring, are truly safer? The long-term outcomes remain statistically underreported. Caution, not compliance, is the prudent stance.
OH MY GOD I CRIED WHEN I READ THIS. I was SO scared to get my wisdom teeth out on warfarin. My last dentist told me to stop it. My cardiologist nearly had a heart attack when I told him. He screamed, "ARE YOU TRYING TO DIE?" I didn't know what to do. I almost canceled. This post? This is the lifeline I needed. I got all four out last week. Used the rinse. No bleeding. No clot. Just me, a soft diet, and a whole lot of relief. THANK YOU. If you're scared - DO NOT STOP. Just bring your INR. Dentists are NOT the enemy.
hi! i'm on xarelto and just had a root canal last week. i was so nervous but my dentist was so chill - she asked if i took it that morning, i said yes, she said "perfect!" and we did it. no big deal. i used the mouthwash thingy and it helped so much. i even forgot to bring my pill bottle but she didn't care. just tell them you're on blood thinners and they'll handle it. you're gonna be okay. i'm a nurse and i used to be scared too - but now i'm like, why did we ever think stopping was a good idea? it's wild. you got this 💪
They say don't stop. But what if your dentist doesn't know what they're doing? What if they're just following a guideline because it's convenient? You're the one with the clot risk. You're the one with the bleeding risk. Who's accountable when it goes wrong? The ADA? The dentist? The pharma rep who funded the study?
DOACs have a half-life of 8–12 hours, so skipping a single pre-op dose creates a pharmacokinetic window that reduces peak plasma concentration without compromising antithrombotic efficacy. This is why the 2023 ACC/AHA guidelines endorse single-dose omission for moderate-risk procedures. Warfarin requires INR titration due to its narrow therapeutic index and CYP450 interactions - which is why it's still the gold standard for complex cases despite its logistical burden.
Just wanted to say this is the most helpful thing I've read all year. I’ve been on Xarelto for 4 years after a DVT. I used to avoid the dentist like the plague. Last month I got a filling and a cleaning - no problem. Dentist gave me the tranexamic rinse and told me to avoid NSAIDs. I used the rinse every 2 hours like they said. Didn’t even need Tylenol. The fear was way worse than the reality. You’re not alone. Just talk to your team. They’ve got your back.
Interesting how the US dental system has evolved. In India, we still see dentists refusing extractions unless the patient stops anticoagulants - even for INR 2.8. It's not just about knowledge gaps. It's cultural. Dentists here fear litigation. They don't have the same institutional backing. Maybe we need a global protocol. Or at least a WHO advisory. This post should be translated. People need to know this isn't just an American thing - it's a medical truth.
So what you're saying is... we're all just lab rats for Big Pharma now? They push DOACs because they're expensive. Then they tell dentists to keep them on because it saves them money on hospitalizations. Meanwhile, your kidneys are slowly dying from the drug and your dentist is just nodding along. Wake up.
bro i got my tooth pulled last week on eliquis and it was fine. dentist gave me some gauze and said "just bite down and don't spit". i did. no bleeding. no drama. dont stop your meds. your doctor knows better than your cousin. also dont drink beer the night before. i did. woke up with a weird taste in my mouth. not worth it.