Dementia isn't a single disease-it's a group of disorders with different causes and symptoms. While Alzheimer's gets the most attention, vascular dementia, frontotemporal dementia (FTD), and Lewy body dementia (LBD) each present unique challenges. Misdiagnosis can lead to harmful treatments, making accurate identification crucial for proper care.
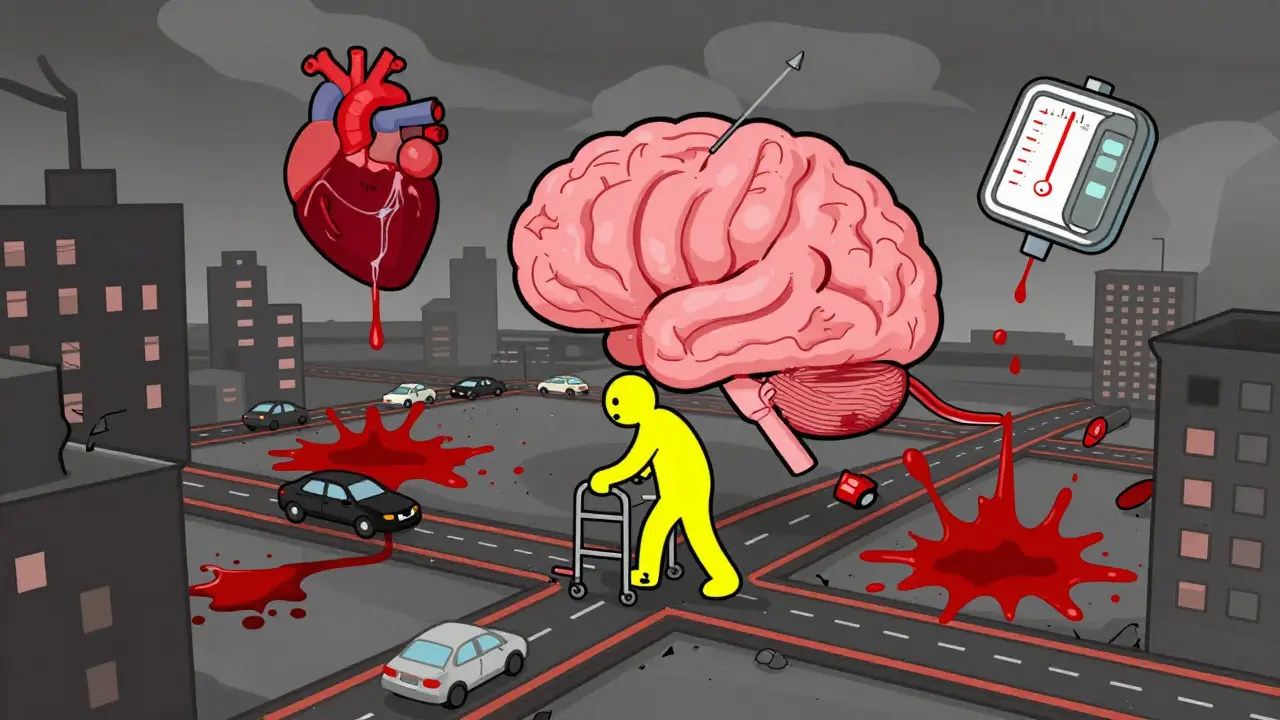
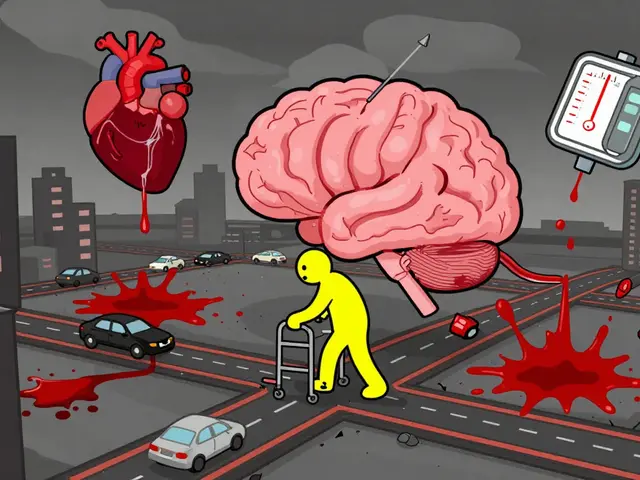
Vascular Dementia
Vascular Dementia is caused by conditions that disrupt blood flow to the brain, such as strokes or chronic high blood pressure. It's the second most common type of dementia after Alzheimer's, affecting about 10% of cases.
This type often follows a stroke or series of small strokes. Symptoms appear suddenly after a vascular event, then stabilize before another decline. Common signs include trouble with planning, memory loss, confusion, and movement problems like unsteady walking. Unlike Alzheimer's, memory issues might not be the first symptom-people often struggle with organization or decision-making first.
Diagnosis relies on brain imaging like MRI or CT scans to spot damaged areas from blocked blood vessels. Doctors also check for risk factors like hypertension, diabetes, or high cholesterol. Treatment focuses on managing these underlying conditions. Controlling blood pressure (targeting below 130/80 mmHg), taking aspirin to prevent clots, and managing diabetes can slow progression. A 65-year-old with uncontrolled hypertension might develop vascular dementia after a minor stroke, but strict blood pressure control can prevent further damage.
Frontotemporal Dementia
Frontotemporal Dementia (FTD) affects the frontal and temporal lobes, which control personality, behavior, and language. It's the most common dementia in people under 60, with symptoms often starting between ages 40-65.
Unlike Alzheimer's, memory remains relatively intact early on. Instead, people show dramatic personality changes: loss of empathy, impulsivity, or social withdrawal. Some develop language problems like struggling to find words or understanding speech. Pathologically, FTD involves abnormal tau or TDP-43 proteins that destroy brain cells in these regions. This leads to shrinkage visible on MRI scans.
Diagnosis combines brain imaging showing frontal/temporal atrophy, neuropsychological tests focusing on executive function (not memory), and ruling out psychiatric conditions. Treatment has no cure, but SSRIs can help with behavioral symptoms. Speech therapy supports those with language difficulties. A 52-year-old might start acting impulsively or losing social graces while keeping sharp memories-this often gets mistaken for depression or bipolar disorder.
Lewy Body Dementia
Lewy Body Dementia involves abnormal deposits of alpha-synuclein protein called Lewy bodies in brain regions controlling thinking and movement. It's the third most common dementia type, affecting 1.4 million Americans (15-20% of cases).
Lewy body dementia has two key features: fluctuating cognition (good and bad days) and visual hallucinations. People might see people or animals that aren't there. They also experience REM sleep behavior disorder (acting out dreams) and Parkinson-like symptoms like muscle rigidity or slow movement. Memory loss isn't usually the first symptom-early on, attention and problem-solving decline more than recall.
Diagnosis uses McKeith criteria requiring at least two core features: cognitive fluctuations, visual hallucinations, REM sleep disorder, or Parkinsonism. Dopamine transporter imaging (DaTscan) helps confirm it. Treatment includes cholinesterase inhibitors like rivastigmine to improve cognition, but antipsychotics are dangerous-up to 75% of LBD patients have severe reactions, including sedation or even death. A person with LBD might see hallucinations one day, then struggle to focus the next, but using the wrong medication can worsen symptoms drastically.
Why Accurate dementia diagnosis Matters
Misdiagnosis is alarmingly common. Lewy body dementia is mistaken for Alzheimer's in 75% of initial cases. Frontotemporal dementia gets misdiagnosed as psychiatric disorders in half of cases. This leads to dangerous treatment errors. For example, antipsychotics used for Alzheimer's hallucinations can trigger life-threatening reactions in LBD patients. Similarly, FTD's behavioral changes might be treated with antidepressants when they're actually neurological.
Accurate diagnosis changes everything. Vascular dementia management focuses on preventing further strokes, while FTD needs behavioral strategies, and LBD requires extreme caution with medications. Proper diagnosis reduces hospitalizations by 30% in LBD cases and ensures safer care. The Alzheimer's Association reports that 40% of Alzheimer's patients also have Lewy bodies, complicating diagnosis-but specialized testing can untangle the mix.
Practical Caregiving Tips
For vascular dementia: Prioritize heart health. Help manage blood pressure, diabetes, and cholesterol. Install grab bars in bathrooms to prevent falls from movement issues. Keep routines simple to reduce confusion.
For frontotemporal dementia: Create structured daily schedules to reduce anxiety. Use clear, short sentences for communication. If personality changes occur, avoid arguing-redirect calmly. Support groups for FTD caregivers are essential, as this type often affects younger people still working or raising families.
For Lewy body dementia: Safety is critical. Remove trip hazards since movement issues increase fall risk. Explain hallucinations matter-of-factly (e.g., "I don't see that, but I'm here with you"). Avoid antipsychotics at all costs. Work with neurologists familiar with LBD for medication adjustments.
Comparison of Dementia Types
| Feature | Vascular Dementia | Frontotemporal Dementia (FTD) | Lewy Body Dementia (LBD) |
|---|---|---|---|
| Primary Cause | Blocked blood vessels from strokes or vascular disease | Abnormal tau or TDP-43 protein buildup | Alpha-synuclein protein deposits (Lewy bodies) |
| Typical Onset Age | 65+ years | 40-65 years | 50+ years |
| Early Symptoms | Planning difficulties, movement issues, step-wise decline | Personality changes, language problems, memory preserved | Visual hallucinations, fluctuating attention, REM sleep disorder |
| Key Diagnostic Tool | Brain MRI showing infarcts | Structural MRI showing frontal/temporal atrophy | DaTscan for dopamine transporters |
| Treatment Focus | Controlling hypertension, diabetes, antiplatelet drugs | SSRIs for behavior, speech therapy | Cholinesterase inhibitors; avoid antipsychotics |
Frequently Asked Questions
Can vascular dementia be prevented?
Yes, up to 40% of vascular dementia cases may be preventable. Controlling high blood pressure (especially in midlife), managing diabetes, quitting smoking, and exercising regularly reduce risk. The SPRINT-MIND trial showed intensive blood pressure control (below 120 mmHg) cut mild cognitive impairment risk by 19% compared to standard treatment.
Why is FTD often mistaken for a mental illness?
FTD's early symptoms-impulsivity, loss of empathy, or obsessive behaviors-resemble psychiatric conditions like depression or bipolar disorder. Up to 50% of FTD cases are initially diagnosed as psychiatric issues. Since FTD affects younger adults still working or raising families, doctors may overlook neurological causes. Neuropsychological testing focusing on executive function (not memory) helps distinguish it.
What makes Lewy body dementia dangerous to treat?
Antipsychotic medications used for Alzheimer's hallucinations can cause severe reactions in LBD patients. Up to 75% experience side effects like extreme sedation, rigid muscles, or even neuroleptic malignant syndrome (a life-threatening condition). Even low doses are risky. Cholinesterase inhibitors are safer for cognitive symptoms, but doctors must avoid all antipsychotics unless absolutely necessary under strict supervision.
How do doctors distinguish LBD from Parkinson's dementia?
The timing of symptoms matters. If dementia symptoms appear before or within one year of Parkinson's motor symptoms (like tremors), it's dementia with Lewy bodies (DLB). If Parkinson's motor symptoms start more than a year before dementia, it's Parkinson's disease dementia (PDD). Both involve Lewy bodies, but DLB has more prominent hallucinations and cognitive fluctuations early on.
Are there blood tests for dementia types?
Blood tests alone can't diagnose dementia types, but they help rule out other causes like vitamin deficiencies. New blood-based biomarkers show promise: plasma GFAP detects vascular injury, and p-tau217 helps identify Alzheimer's. For LBD, alpha-synuclein tests are in development but not yet routine. Diagnosis still relies on imaging, symptoms, and clinical evaluation.
This is a well-researched piece. I especially appreciate the emphasis on controlling blood pressure for vascular dementia. It's a simple but crucial step.
This is too vague. Needs more specifics on treatment options.
Prevent vascular dementia: control BP. Done.
Ugh, another article about dementia. It's all doom and gloom. No one ever talks about the emotional toll on caregivers. Just another waste of time.
Wow, this article is a classic example of oversimplification. Vascular dementia isn't just about strokes; small vessel disease is a huge factor that's completely ignored here. The table says "blocked blood vessels from strokes or vascular disease" but doesn't differentiate between large vessel and small vessel. Also, the treatment section says controlling hypertension is key, but in reality, many patients have resistant hypertension that requires multiple meds. The article mentions "targeting below 130/80 mmHg" but doesn't address how hard it is to achieve in elderly patients with comorbidities. FTD is misdiagnosed as psychiatric disorders, but the article doesn't mention the role of genetic testing-like mutations in MAPT or GRN genes. For LBD, the DaTscan is useful but expensive and not accessible everywhere. The article claims antipsychotics are dangerous for LBD, which is true, but doesn't mention alternatives like quetiapine at low doses for severe psychosis. Also, the comparison table is misleading; it says LBD has "visual hallucinations" as an early symptom, but in reality, hallucinations often come later. The article's "practical caregiving tips" are too generic-no specific advice for managing fluctuating cognition. For example, how to handle sudden confusion episodes. And why no mention of non-pharmacological interventions like cognitive stimulation therapy for FTD? The Alzheimer's Association statistic about 40% of Alzheimer's patients also having Lewy bodies is mentioned but not contextualized. This article is a missed opportunity to provide nuanced information. It's too surface-level for a topic this complex.
Good info. Important to get the right diagnosis early.
The comparison table is useful. However, I'd like to see more on how to differentiate LBD from Parkinson's dementia, as that's a common point of confusion.
Great breakdown! I've been dealing with a family member with FTD. The behavioral changes are tough, but structured schedules help. Love the tips for caregivers.
Actually, the timing difference between DLB and PDD is key. If dementia starts within a year of motor symptoms, it's DLB. Otherwise PDD. But the article mentions it briefly.
This is really helpful! 🌟 Especially the part about LBD and antipsychotics. So important to avoid those meds. Hope more people know this. 💡
Wow, this article really breaks it down. Like, who knew antipsychotics could kill LBD patients? 🤦♂️ Maybe doctors should read this before prescribing.
This article ignores American healthcare realities Insurance wont cover DaTscans We need cheaper solutions Stop overcomplicating things
Pharmaceutical companies are pushing dementia labels to sell drugs. They hide natural cures. This whole thing is a scam.
Yeah, I've seen this with my grandma. Vascular dementia is tough, especially when they don't catch it early. Like, high blood pressure control is key, but sometimes people don't take meds properly. Maybe more education needed on that. Also, the article mentions stroke-related vascular dementia, but small vessel disease is a big factor too-like white matter hyperintensities on MRI. FTD's personality changes are often mistaken for depression, but it's neurological. The SPRINT-MIND trial showed intensive BP control reduces cognitive decline, but it's hard to implement in real life. For LBD, the DaTscan is gold standard but expensive. And antipsychotics are dangerous, but some doctors still prescribe them. The comparison table is helpful, but missing info on how to manage fluctuating cognition in LBD. Caregivers need more support-like respite care options. Also, the article says 'step-wise decline' for vascular dementia, but in practice, it's often gradual. Maybe because of multiple small strokes over time. And why no mention of sleep apnea's role in vascular dementia? It's a common comorbidity. The Alzheimer's Association stats are good, but they don't talk about disparities in diagnosis rates among different ethnic groups. For example, African Americans have higher vascular dementia rates but less access to specialists. This article is a good start, but needs more depth on real-world challenges and inequities. Also, the 'practical caregiving tips' are too vague. Like, how to handle sudden confusion episodes in LBD? Need specific strategies. And for FTD, how to communicate when language skills decline. Maybe use visual aids or apps. The table is useful, but more details on treatment options would help. Like, cholinesterase inhibitors for LBD, but not for vascular. Also, non-pharmacological interventions for FTD behavior issues. Overall, good info but needs more nuance.