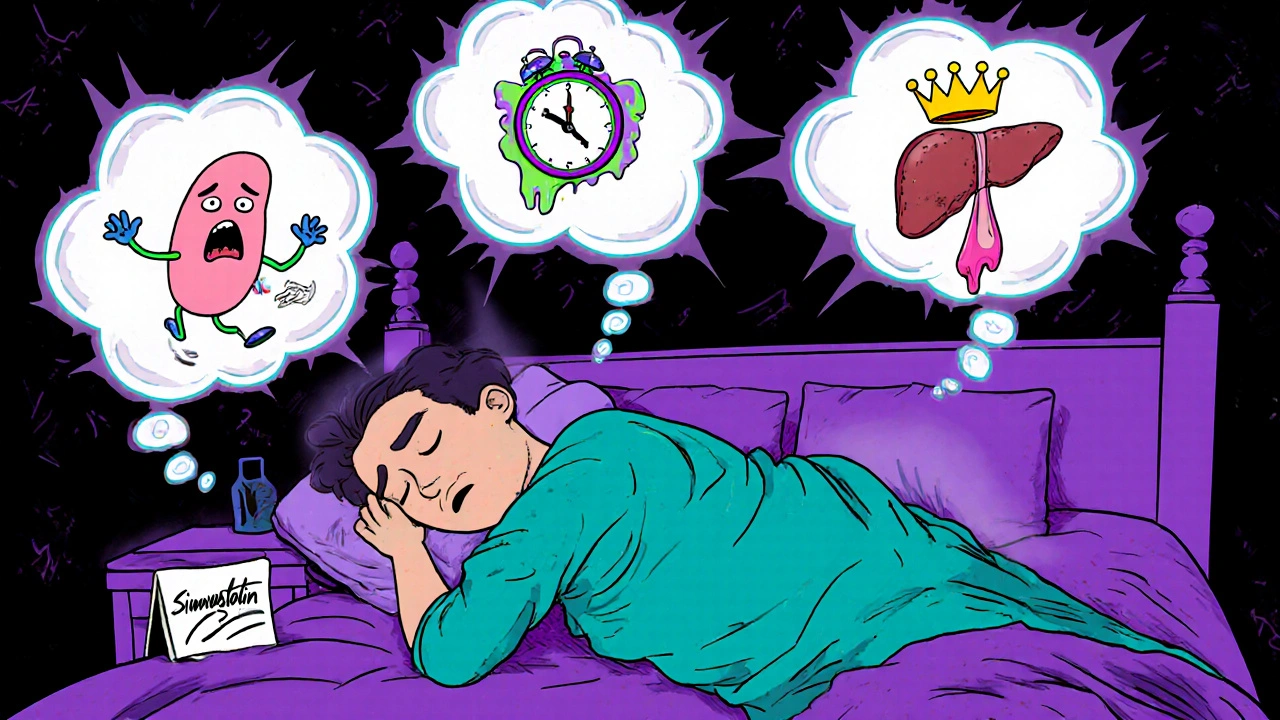
Statin Sleep Side Effects: What You Need to Know About Insomnia and Fatigue
When you take a statin, a class of drugs used to lower LDL cholesterol and reduce heart attack risk. Also known as HMG-CoA reductase inhibitors, they’re among the most prescribed medications in the world. But for some, the benefits come with a hidden cost: disrupted sleep and unexplained tiredness. If you’ve been on a statin and suddenly can’t fall asleep, wake up at 3 a.m., or feel drained even after a full night’s rest, you’re not imagining it. Research from the Journal of Clinical Sleep Medicine and patient reports consistently link statins to sleep disturbances—especially with lipophilic types like simvastatin and atorvastatin.
Why does this happen? Statins reduce cholesterol, which your body needs to make melatonin—the hormone that tells your brain it’s time to sleep. Lower cholesterol means less raw material for melatonin production. Some studies also suggest statins may affect muscle energy production, leading to fatigue that feels like exhaustion even without physical exertion. It’s not just in your head. A 2021 analysis of over 12,000 patients found that those on statins were 20% more likely to report insomnia than those not taking them. And it’s not always the same drug: rosuvastatin seems to cause fewer sleep issues than simvastatin, while pravastatin has the lowest reported rate of sleep-related side effects.
This isn’t just about tossing and turning. Poor sleep from statins can worsen other conditions—like high blood pressure, diabetes, and even depression. And if you stop the medication because of sleep problems, you might be trading one risk for another. The good news? You don’t have to live with it. Switching to a different statin, taking your dose in the morning instead of at night, or adding a low-dose melatonin supplement (after checking with your doctor) can help. Some people find relief by pairing their statin with ezetimibe, a non-statin cholesterol drug that works differently and rarely causes sleep issues. Others benefit from bempedoic acid, a newer oral option that lowers LDL without crossing the blood-brain barrier, making it less likely to interfere with sleep hormones.
If you’re struggling with sleep or fatigue while on a statin, the first step isn’t quitting—it’s talking to your doctor about your symptoms and options. You might not need to stop the drug. You might just need to change which one you’re taking, when you take it, or add a simple support strategy. The posts below dive into real cases, comparisons of statin alternatives, and practical steps to reclaim your sleep without sacrificing heart health. You’ve got choices. Let’s look at what works.
Statins and Sleep Problems: Can Cholesterol Meds Cause Insomnia and Vivid Dreams?
Can statins cause insomnia or vivid dreams? Learn which statins are most likely to disrupt sleep, how to tell if it's the medication, and what to do next-backed by clinical studies and patient experiences.