Millions of people take statins every day to lower their cholesterol and protect their hearts. But if you’ve been waking up in the middle of the night with your mind racing or having dreams so vivid they feel real, you’re not alone. Many patients report sleep issues after starting statins-and some swear their dreams got weirder the moment they swallowed that pill. So is there a real link between statins and sleep problems? Or is it all in your head?
What the Science Actually Says
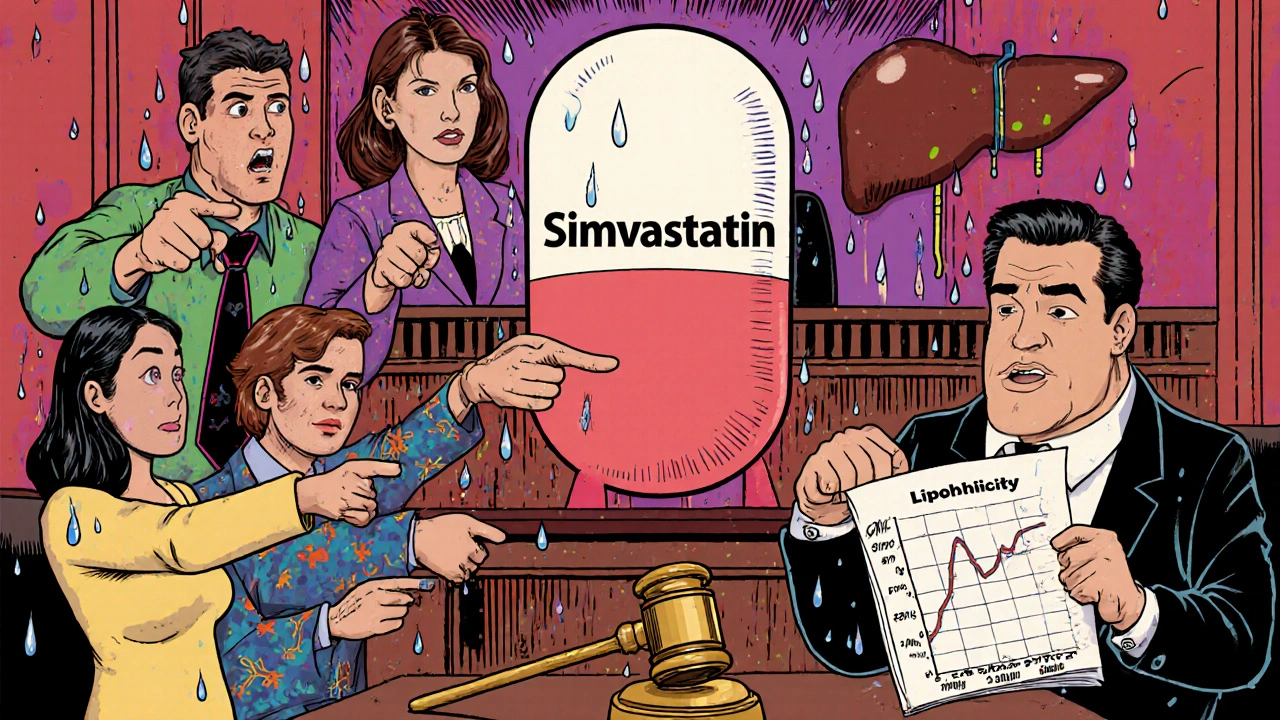
The truth? It’s messy. Some studies say statins don’t affect sleep. Others say they do-especially certain types. The confusion comes down to one big factor: lipophilicity. That’s just a fancy word for how easily a drug can cross into your brain.
Statins like simvastatin, lovastatin, and atorvastatin are lipophilic. That means they slip through the blood-brain barrier more easily. Hydrophilic statins-like pravastatin and rosuvastatin-don’t cross as easily. And here’s the kicker: research shows people taking lipophilic statins report more sleep trouble.
In a 2007 study led by Dr. Beatrice Golomb, 1,016 adults were given either simvastatin, pravastatin, or a placebo. Those on simvastatin reported significantly worse sleep quality than the others. Pravastatin? No different from the placebo. Another analysis of FDA reports found simvastatin was linked to over twice the number of sleep disturbance reports compared to other statins. Rosuvastatin showed a moderate link, but atorvastatin? Almost no connection.
Meanwhile, a massive 2018 study of 10,000 people found people taking atorvastatin had fewer sleep problems than those on placebo. How? That’s where the nocebo effect comes in. If you’ve read online that statins cause nightmares, your brain might start looking for them-even if the drug isn’t the cause.
Why Vivid Dreams Happen (Maybe)
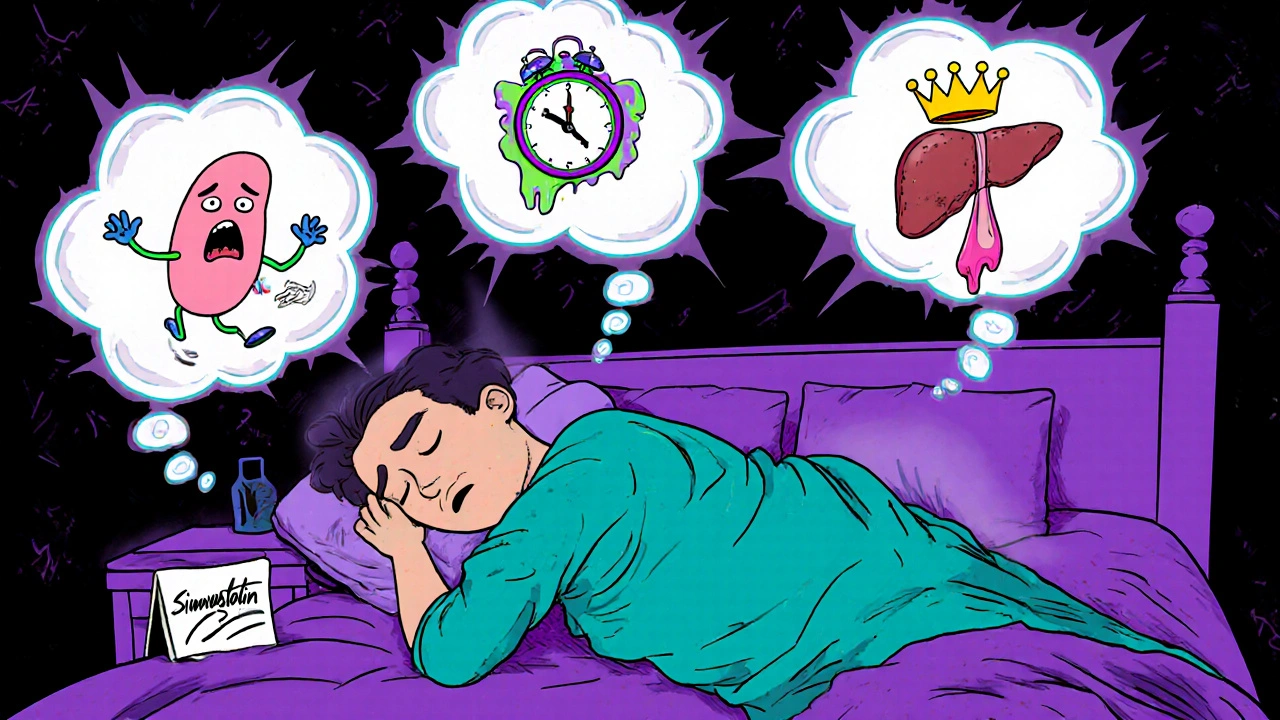
Statins block an enzyme called HMG-CoA reductase, which your body uses to make cholesterol. But that same enzyme is involved in making other compounds too-including those that affect brain chemicals like serotonin and melatonin. These are the very chemicals that regulate sleep cycles and dreaming.
When your brain’s chemistry shifts-even slightly-it can disrupt REM sleep, the stage where dreams are most intense. That’s why some people report sudden, lifelike dreams after starting simvastatin. One Reddit user wrote: “Switched from atorvastatin to pravastatin and my crazy dreams stopped in three days.” That’s not rare. Case reports like this pop up all the time.
It’s not just dreams, either. Some people report trouble falling asleep, waking up too early, or feeling unrested even after 8 hours. These aren’t just “stress” complaints. They’re real, measurable changes in sleep architecture.
The Muscle-Sleep Connection
Here’s something most people don’t realize: sleep problems might not be coming from the statin itself-but from muscle pain.
Statin-Associated Muscle Symptoms (SAMS) are common. Aching legs, tired arms, stiffness. These symptoms often get worse at night. And when you’re in pain, you can’t sleep well. A 2024 study found that when patients stopped statins because of muscle pain, their sleep quality improved dramatically: fewer nighttime awakenings, less time lying awake, better overall rest.
So if you’re having trouble sleeping, ask yourself: Is it the dream? Or is it the ache? Sometimes, the two go hand in hand.
Which Statins Are Most Likely to Cause Sleep Issues?
Not all statins are created equal. Here’s what the data shows:
| Statin | Lipophilicity | Sleep Disturbance Risk | Notes |
|---|---|---|---|
| Simvastatin | High | High | Most commonly linked to insomnia and vivid dreams in studies and patient reports |
| Lovastatin | High | High | Early case reports linked it to sleep loss-some patients lost 1-3 hours per night |
| Rosuvastatin | Moderate | Moderate | Some reports, but less than simvastatin. Still flagged in FDA data |
| Atorvastatin | Moderate | Low | Large trials show no increase vs. placebo; may even improve sleep in some |
| Pravastatin | Low | Very Low | Consistently shown to have no effect on sleep compared to placebo |
| Pitavastatin | Low | Very Low | Minimal reports; considered safe for sleep-sensitive patients |
If you’re on simvastatin or lovastatin and having sleep issues, switching to pravastatin or pitavastatin might help. One study showed that 72% of patients who switched from a lipophilic statin to a hydrophilic one saw their sleep problems improve within 4 weeks.
What You Can Do Right Now
If you’re on a statin and noticing sleep problems, don’t panic. Don’t stop cold turkey. But do take action.
- Track your sleep. Use a simple journal: note when you go to bed, when you wake up, and whether you had strange dreams. Do this for 2 weeks.
- Check your timing. Some people find taking statins in the morning instead of at night helps-especially if they’re on a lipophilic statin. Your liver makes most cholesterol at night, but your brain might be more sensitive to the drug’s effects if it’s active while you’re sleeping.
- Rule out muscle pain. Are your legs cramping? Do you feel stiff in the morning? If yes, that might be the real culprit behind your sleep loss.
- Talk to your doctor. Ask about switching to pravastatin or pitavastatin. These are just as effective at lowering cholesterol but much less likely to mess with your sleep.
- Give it time. If you do switch, give it 3-4 weeks. Sleep patterns don’t fix overnight.
And if you’re still unsure? Try a short, supervised pause. Under medical supervision, stopping your statin for 2-4 weeks can tell you if it’s the cause. If your sleep improves, you’ve got your answer. If not? The problem’s probably elsewhere-stress, caffeine, sleep apnea, or something else.
Don’t Skip the Statin-Just Switch Smartly
Statins save lives. They cut heart attacks and strokes by up to 22% for every 1 mmol/L drop in LDL cholesterol. That’s not small. If you’ve had a heart attack or have high risk, stopping statins without a plan is dangerous.
But you don’t have to suffer sleepless nights to stay healthy. There are better options. Pravastatin works just as well for most people. Pitavastatin is newer but just as effective. Even low-dose rosuvastatin might be fine if you’re not sensitive to it.
The goal isn’t to avoid statins. It’s to find the one that works for you-without stealing your sleep.
What’s Next in Research?
Scientists are still digging. A major trial called NCT04567891 is currently testing whether cognitive behavioral therapy for insomnia (CBT-I) can help people stay on statins-even if they have sleep issues. Results are expected in mid-2025.
Other studies are looking at genetics. Some people may be more prone to statin-related sleep problems because of how their bodies process the drugs. That could lead to personalized prescriptions in the future.
For now, the best advice is simple: if your sleep changed after starting a statin, it’s worth investigating. Don’t assume it’s stress. Don’t assume it’s all in your head. And don’t assume you have to live with it.
Can statins really cause vivid dreams?
Yes, some people report vivid, intense, or even disturbing dreams after starting certain statins-especially simvastatin and lovastatin. These drugs can cross into the brain and affect neurotransmitters linked to REM sleep, where dreaming happens. While not everyone experiences this, it’s a documented side effect in clinical studies and patient reports.
Which statin is least likely to affect sleep?
Pravastatin and pitavastatin are the least likely to cause sleep problems. Both are hydrophilic, meaning they don’t cross the blood-brain barrier easily. Multiple studies show they have no significant impact on sleep quality compared to placebo. If you’re having trouble sleeping on a statin, switching to one of these is often the first recommended step.
Should I stop taking statins if I have insomnia?
No-not without talking to your doctor. Statins reduce your risk of heart attack and stroke significantly. Instead of stopping, work with your provider to switch to a different statin, like pravastatin, or adjust your dose and timing. A short, supervised break (2-4 weeks) can help determine if the statin is the cause.
How long does it take for sleep to improve after switching statins?
Most people notice improvement within 2-4 weeks after switching to a hydrophilic statin like pravastatin. Some report better sleep in just a few days, especially if vivid dreams were the main issue. If muscle pain was contributing to poor sleep, improvements may take longer-up to 6 weeks.
Can taking statins in the morning help with sleep?
For some people, yes. Even though cholesterol production peaks at night, taking a lipophilic statin like simvastatin in the morning may reduce its impact on brain chemistry during sleep. This isn’t a guaranteed fix, but it’s a simple, low-risk adjustment to try before switching medications.
Are sleep problems from statins permanent?
No. If statins are causing your sleep issues, symptoms typically resolve within weeks of stopping or switching medications. In clinical case reports, patients who discontinued simvastatin or switched to pravastatin saw their sleep return to normal. The effect is not permanent, but it can be distressing while it lasts.
Final Thought
Statins aren’t the enemy. But they’re not magic bullets either. They’re powerful tools-and like all powerful tools, they come with trade-offs. If your sleep’s been off since you started one, it’s not something to ignore. It’s a signal. Listen to it. Talk to your doctor. Try a switch. Give your body time to adjust. You don’t have to choose between a healthy heart and a good night’s sleep. There’s a statin out there that lets you have both.
I switched from simvastatin to pravastatin last year after months of nightmare fuel. One night I dreamed I was being chased by a giant floating toaster. Not metaphorical. Literal. Then I switched meds and slept like a baby. No more weird dreams, no more anxiety wakes. Just peace.
Also, my legs stopped aching. Who knew?
YES!! This is so real. I was on atorvastatin and thought I was losing my mind. Dreams where I was flying over cities made of cheese? I didn’t even know that was possible. Switched to pravastatin and boom - normal sleep returned. My wife said I stopped screaming in my sleep. She was happy. I was relieved.
Don’t suffer. Talk to your doc. You’re not crazy.
:)
Statins cause nightmares and people are shocked Really You take a drug that blocks cholesterol in your brain and expect to dream about your ex holding a chainsaw No wonder you’re confused
Wow. A 2007 study? And you're still treating this like a mystery? The mechanism is literally in the name: lipophilic = brain penetration. You don't need a 10,000-person trial to figure out that if a drug gets into your CNS, it affects your CNS. Basic pharmacology. Stop pretending this is controversial.
lol statins make you have dreams?? bro i had a dream i was a dolphin last week and i dont even take meds. maybe its the wine. or the fact that you watch too much netflix before bed. also pravastatin? sounds like a vitamin for cows
Just want to say - this is such a helpful breakdown. I’ve been on simvastatin for 3 years and thought I was just stressed. Turns out I was having 3-4 vivid dreams a night, waking up exhausted. Switched to pitavastatin 3 weeks ago and honestly? I forgot what it felt like to sleep through the night. No more dreams about my high school math teacher yelling at me in a submarine. Life is good now.
Thanks for the clear info. You saved my sanity.
OMG I thought I was the only one!! I was having dreams where I was trapped in a mirror version of my house and my cat was speaking in Latin. I told my doctor and she laughed. Like I was joking. I cried. Then I switched to pravastatin and my dreams went back to normal - just boring ones about grocery lists and being late to work. I miss the weird ones but I’ll take normal sleep any day
So I’ve been on rosuvastatin for a while and I did notice my sleep got weird like 6 months in - I’d wake up at 3am feeling super alert like my brain was on full blast. I thought it was caffeine or my phone but then I read this and it made so much sense. I didn’t even know statins could get into the brain. I’m gonna ask my doc about switching to pravastatin. I’m not scared of meds but I’m scared of not sleeping. I just want to rest. I’m so tired all the time. Maybe it’s not stress. Maybe it’s the pill. I’m gonna try the morning dose first. Thanks for explaining it so simply.
Statins and sleep? This is the most important thing I’ve read all year. I’ve been telling people for months that my dreams got intense after starting atorvastatin. They said I was overreacting. Now I’ve got science on my side. I’m switching to pravastatin next week. If you’re reading this and you’re struggling - you’re not alone. Your sleep matters. Your brain matters. Don’t ignore it.
Why are you even taking statins? In India we dont need them unless you are 70 and have 3 heart attacks already. You eat too much bread and sugar. Stop blaming the medicine. Fix your diet. Then you wont need pills or have weird dreams. Also you sleep too much anyway
Thank you for writing this with so much care. I’m a nurse and I’ve seen so many patients suffer silently because they think sleep issues are ‘just aging’ or ‘stress.’ This post gives them real, actionable info. I’m sharing it with my whole team. Also - pravastatin is a game changer. One patient went from 4 wake-ups a night to 1 after switching. No side effects. No drama. Just better sleep. You’re doing good work.
Interesting how the nocebo effect is mentioned but not emphasized enough. In my clinic, patients who read about statin side effects online are way more likely to report them - even if they’re on placebo. That doesn’t mean the effect isn’t real for some - but it does mean we need to be careful about how we talk about it. Education matters.
Wait so if I switch to pravastatin will my dreams go back to normal? I had one where I was a ghost haunting my own apartment and I couldn’t leave. I think I’m losing my mind. Or is this just my brain being dramatic? I don’t know anymore. I just want to sleep without seeing my ex in a shark costume.
Yes. I promise. I had the exact same dream. Except mine was my ex in a toaster. Switched meds. Three days later - silence. No ghosts. No sharks. Just me, my blanket, and 8 hours of peace. You got this.