Global HCV Elimination: How Medications, Access, and Policy Are Ending Hepatitis C
When we talk about global HCV elimination, the worldwide effort to stop hepatitis C virus transmission and cure all infected people by 2030. Also known as hepatitis C eradication, it’s not just about pills—it’s about making sure those pills reach the people who need them, no matter where they live. For decades, hepatitis C was a silent killer. Many didn’t know they had it until their liver was badly damaged. But today, we have medicines that cure over 95% of cases in just 8 to 12 weeks. These are called direct-acting antivirals, a new class of oral drugs that target the hepatitis C virus directly, without the harsh side effects of older treatments. They’re not expensive like they used to be. Thanks to generic manufacturers—especially in India—these drugs now cost less than $50 a course in many countries.
But curing individuals isn’t enough. global HCV elimination, the worldwide effort to stop hepatitis C virus transmission and cure all infected people by 2030. Also known as hepatitis C eradication, it’s not just about pills—it’s about making sure those pills reach the people who need them, no matter where they live. For decades, hepatitis C was a silent killer. Many didn’t know they had it until their liver was badly damaged. But today, we have medicines that cure over 95% of cases in just 8 to 12 weeks. These are called direct-acting antivirals, a new class of oral drugs that target the hepatitis C virus directly, without the harsh side effects of older treatments. They’re not expensive like they used to be. Thanks to generic manufacturers—especially in India—these drugs now cost less than $50 a course in many countries.
That’s why HCV screening, the process of testing people for hepatitis C infection, often through simple blood tests, to identify those who need treatment. is so critical. You can’t treat what you don’t find. In places like Egypt and Georgia, mass screening programs in pharmacies and community clinics helped cut infection rates by half in just five years. In the U.S., one-time testing for baby boomers saved thousands of lives. But in many low-income countries, testing is still rare. People don’t get tested because they don’t know they’re at risk, or because clinics are too far, or because the test costs more than a meal.
And here’s the truth: global HCV elimination isn’t a medical challenge anymore. It’s a systems problem. It’s about training nurses to give tests in rural villages. It’s about getting governments to drop import taxes on generics. It’s about stopping stigma so people feel safe getting checked. It’s about linking people who test positive to care—fast. We’ve had the tools for years. What’s missing is the will to use them everywhere, not just where it’s easy.
What you’ll find in the posts below are real stories about how this plays out: from how India became the pharmacy of the world supplying these cures, to how people on low incomes access treatment, to how drug patents and delays still block access in some places. You’ll see how one pill can change a life—and how policy, pricing, and access decide who gets that chance.
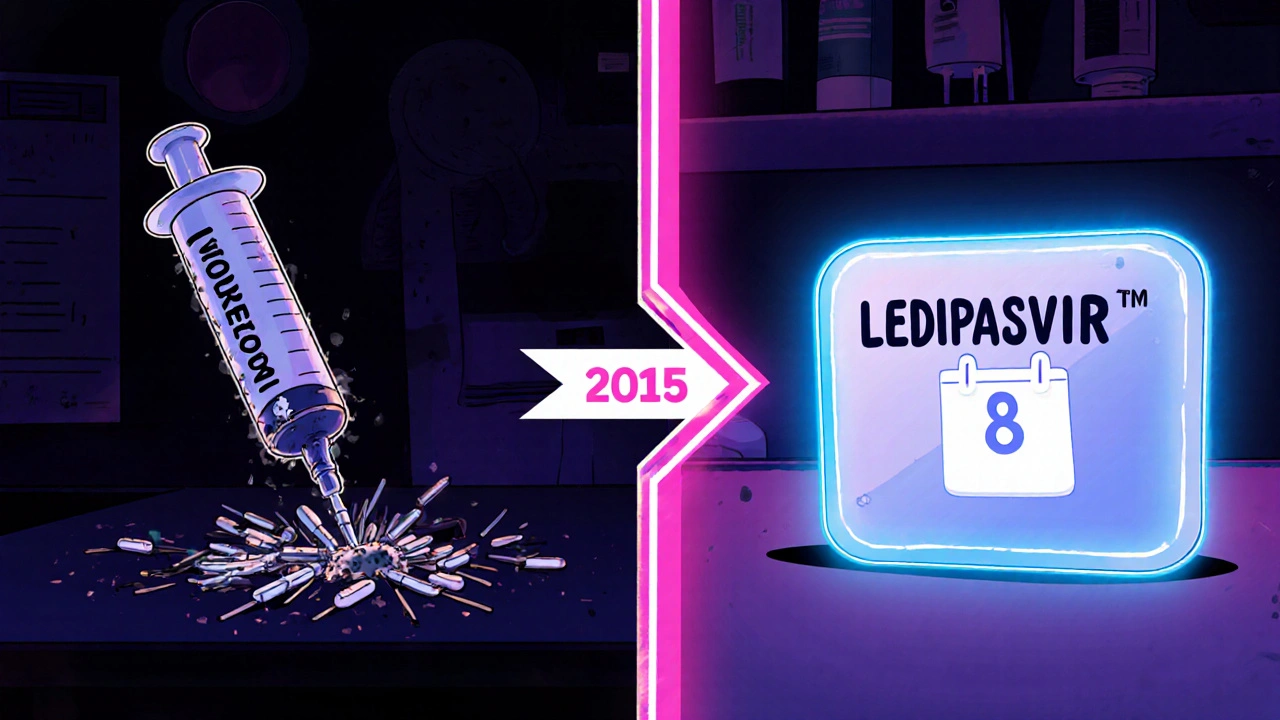
Ledipasvir’s Impact on Global Hepatitis C Treatment
Explore how Ledipasvir transformed hepatitis C therapy worldwide, boosting cure rates, shaping WHO elimination goals, and what challenges and future prospects lie ahead.