Ledipasvir is a direct‑acting antiviral (DAA) that targets the NS5A protein of hepatitis C virus (HCV). Since its FDA approval in 2014, the drug has become a cornerstone of modern HCV therapy, especially when paired with sofosbuvir in the fixed‑dose combination known as Harvoni. This article walks through how Ledipasvir changed the global treatment landscape, why clinicians and public‑health officials are buzzing about it, and what the next few years might look like for patients worldwide.
What Ledipasvir Is and How It Works
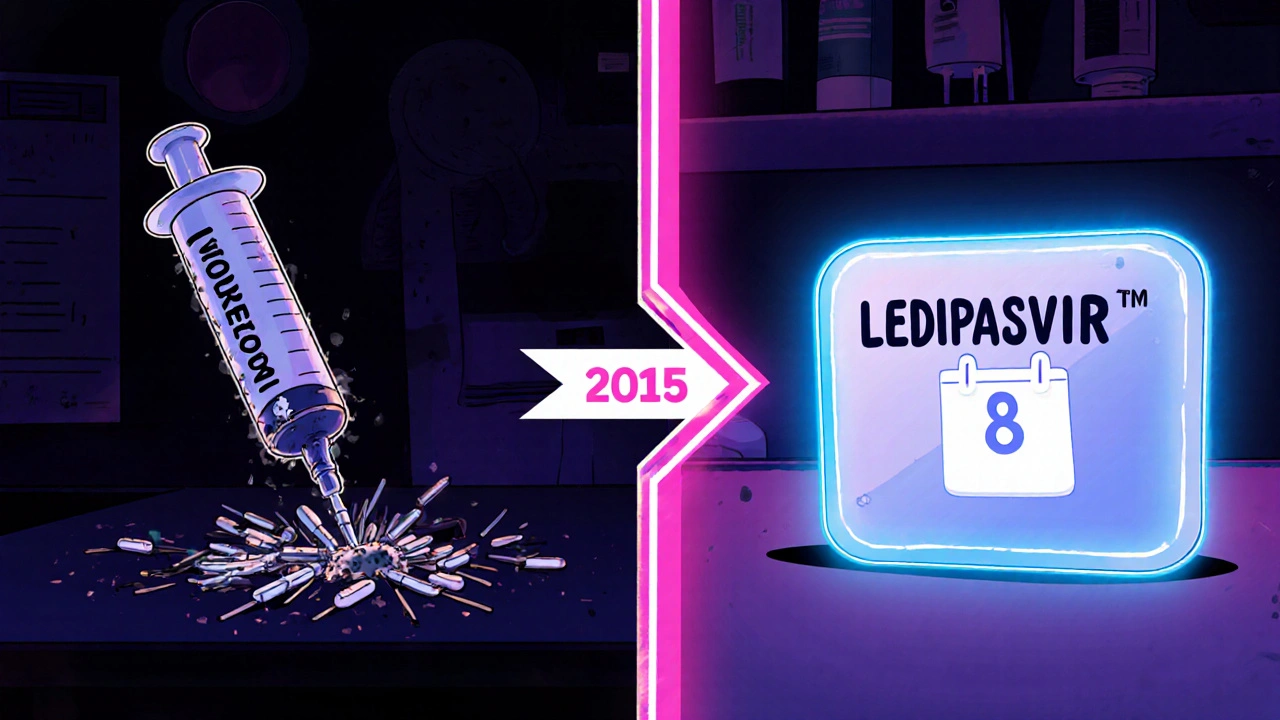
Ledipasvir belongs to the class of direct‑acting antivirals (DAAs). Unlike the interferon‑based regimens that required weekly injections and caused flu‑like side effects, DAAs act directly on viral proteins to halt replication. Specifically, Ledipasvir binds to the NS5A replication complex, destabilizing the viral RNA‑polyprotein processing and preventing new virions from forming.
From Clinical Trials to Real‑World Success
The pivotal ION‑1, ION‑2, and ION‑3 trials enrolled over 3,000 treatment‑naïve and -experienced patients with HCV genotype 1 - the most common genotype worldwide. Across these studies, Ledipasvir‑sofosbuvir achieved sustained virologic response (SVR) rates of 94‑99 % after just eight weeks of therapy, with fewer adverse events than older regimens. Real‑world data from the HCV‑RealWorld Registry (2020‑2024) confirmed SVR > 96 % across diverse populations, including patients with cirrhosis and those on opioid‑substitution therapy.
Why the Global Landscape Shifted Overnight
The introduction of Ledipasvir‑sofosbuvir effectively turned HCV from a chronic, hard‑to‑treat infection into a curable disease with a short, all‑oral course. Six key changes illustrate the impact:
- Shorter treatment duration: eight‑week courses replaced 24‑48‑week interferon protocols.
- Higher cure rates: SVR climbed from ~50 % with interferon‑ribavirin to >95 % with DAAs.
- Improved tolerability: side‑effects like depression and anemia dropped dramatically.
- Simplified logistics: no injections, fewer clinic visits, and easy adherence.
- Expanded eligibility: even patients with decompensated cirrhosis or post‑liver‑transplant can be treated.
- Price‑driven negotiations: generic versions entered markets in India, Egypt, and Brazil, driving down costs to <$500 per 12‑week course in many low‑income settings.

Comparison: Ledipasvir/Sofosbuvir vs. Interferon‑Based Therapy
| Attribute | Ledipasvir/Sofosbuvir (Harvoni) | Interferon + Ribavirin |
|---|---|---|
| Typical Duration | 8-12 weeks | 24-48 weeks |
| SVR (cure) Rate | 94-99 % | 45-55 % |
| Route of Administration | Oral tablets | Weekly subcutaneous injection + oral ribavirin |
| Common Side Effects | Fatigue, headache (mild) | Depression, anemia, flu‑like symptoms |
| Contra‑indications | Severe renal impairment (eGFR < 30) | Autoimmune disease, uncontrolled psychiatric disorders |
| Cost (US, 2023) | ≈ $30,000 for 12‑week course (brand) | ≈ $25,000-$30,000 for full course |
Driving the WHO’s Goal of HCV Elimination by 2030
The World Health Organization set an ambitious target to eliminate HCV as a public health threat by 2030 - that means a 90 % reduction in new infections and a 65 % drop in mortality. Ledipasvir‑based regimens are a linchpin of this effort. According to the WHO 2024 progress report, countries that adopted DAA‑first policies (including Ledipasvir) saw a 40 % decline in HCV incidence within five years, compared to a 10 % decline in regions still reliant on interferon.
Regional Adoption and Access Challenges
While high‑income nations quickly integrated Ledipasvir into national guidelines (e.g., the United States’ AASLD/IDSA 2022 update, the European Association for the Study of the Liver 2023), lower‑income regions faced pricing and licensing hurdles. Two mechanisms helped bridge the gap:
- Voluntary licensing: Gilead granted licenses to Indian manufacturers, enabling affordable generics. Egypt’s national program, for example, purchased 150,000 treatment courses at <$150 each.
- International procurement: The Global Fund and UNITAID pooled demand, negotiating bulk discounts that lowered the price ceiling for Sub‑Saharan Africa.
Even with these measures, access gaps remain in parts of Southeast Asia where regulatory delays keep generics off the market.

Future Outlook: Resistance, Next‑Gen DAAs, and Combination Strategies
Resistance‑associated substitutions (RAS) to NS5A inhibitors can emerge, especially in patients with prior DAA exposure. However, studies like the 2025 RESIST‑HCV trial show that adding a third agent (e.g., velpatasvir) restores cure rates above 95 % even in RAS‑positive cases. Researchers are also exploring pan‑genotypic regimens that combine Ledipasvir‑like molecules with novel polymerase inhibitors, aiming for a "one‑pill‑for‑all" solution.
Practical Guidance for Clinicians
When deciding whether to prescribe Ledipasvir‑sofosbuvir, clinicians should follow these steps:
- Confirm HCV genotype (Ledipasvir works best for genotype 1 and 4).
- Assess liver fibrosis stage (F0‑F3 patients can use the 8‑week regimen; F4 may need 12 weeks).
- Check renal function; avoid if eGFR < 30 mL/min/1.73 m².
- Review drug‑drug interactions - Ledipasvir is a substrate of P‑gp and BCRP; avoid concomitant use with strong inducers such as rifampin.
- Educate patients on adherence - missed doses reduce SVR by ~5 %.
Adhering to the AASLD/IDSA 2022 guidance ensures optimal outcomes and minimizes the risk of resistance.
Key Takeaways
- Ledipasvir turned HCV into a curable disease with short, well‑tolerated oral therapy.
- Global cure rates jumped dramatically, accelerating WHO’s elimination goals.
- Access has expanded through generic licensing and bulk procurement, yet regional gaps persist.
- Future regimens will likely blend Ledipasvir‑like agents with next‑gen DAAs to cover all genotypes and overcome resistance.
What is the cure rate of Ledipasvir/Sofosbuvir for genotype 1 HCV?
Clinical trials and real‑world registries report sustained virologic response (SVR) rates of 94‑99 % after an eight‑week course for treatment‑naïve genotype 1 patients.
Can Ledipasvir be used in patients with advanced liver disease?
Yes. For compensated cirrhosis (Child‑Pugh A‑B) an extended 12‑week regimen is recommended. Decompensated patients may need a ribavirin‑free combination that includes a second‑generation DAA.
How does the cost of generic Ledipasvir compare to the brand version?
In high‑volume markets such as India and Egypt, generic Ledipasvir‑sofosbuvir courses are priced between $150‑$300, a fraction of the $30,000 brand price in the United States.
What are the most common drug interactions with Ledipasvir?
Strong P‑gp or BCRP inducers like rifampin, St. John’s wort, and carbamazepine can lower Ledipasvir plasma levels. Dose adjustments are not recommended; instead, avoid co‑administration.
Is Ledipasvir effective against HCV genotypes other than 1?
Ledipasvir shows high potency against genotype 4 and moderate activity against genotype 2 and 3 when combined with other DAAs. For pan‑genotypic needs, clinicians often choose sofosbuvir‑velpatasvir instead.
The transition to all‑oral regimens like ledipasvir‑sofosbuvir really streamlined patient management. With SVR rates above 95 %, clinicians can feel more confident prescribing shorter courses. It also reduced the burden on infusion centers.
This breakthrough really lifts hope for many people.
From a pharmacokinetic standpoint, ledipasvir exhibits a high hepatic extraction ratio and synergizes with sofosbuvir’s NS5B polymerase inhibition, consequently suppressing the replication complex across genotypes 1‑4 🚀💊 the pangenotypic potential is further enhanced by nucleotide analog incorporation pathways – a true paradigm shift in antiviral therapy.
Seriously, these hype‑filled press releases sound like marketing fluff. The real‑world data still shows pockets of resistance and the economics are a nightmare for public health budgets.
It is incumbent upon us to scrutinize the underlying motivations of pharmaceutical conglomerates; the accelerated approval pathways may conceal long‑term safety signals, and the proliferation of generics in certain regions raises concerns about regulatory oversight and potential data manipulation.
While vigilance is prudent, the post‑marketing surveillance data for ledipasvir‑sofosbuvir have not indicated any emergent hepatotoxicity beyond the established safety profile. Moreover, the cost‑effectiveness analyses conducted by independent health economics groups corroborate its favorable value proposition.
The so‑called “favorable value proposition” is a mirage painted by stakeholders desperate to keep profits flowing; patients are left grappling with hidden co‑pay cliffs while the narrative glorifies a cure that masks ongoing surveillance gaps.
Oh absolutely, a single sentence can capture the enormity of this medical revolution-if only optimism were a substitute for data, right?
We cant turn a blind eye to the ethicalImplications of making such oodles of profit off a disease that once crippled so many lives; it's a reminder that we must keep the cure accessible for all, not just the privileged few.
Exactly! 🌟
The introduction of ledipasvir‑sofosbuvir marked a watershed moment in the fight against hepatitis C. By condensing therapy to eight weeks, it removed a major barrier for patients with limited healthcare access. The high SVR rates observed in both trial and real‑world cohorts have translated into measurable reductions in liver‑related morbidity. Health ministries in Egypt and Brazil have incorporated the regimen into national elimination programs, driving down prevalence. Meanwhile, the emergence of quality‑assured generics has lowered the price per treatment course to under $500 in some markets. This price compression has enabled NGOs to expand screening campaigns in underserved regions. However, disparities remain, as high‑income countries still negotiate pricing based on bulk purchasing power. Insurance formularies in the United States often impose step‑therapy requirements that delay initiation. The pharmacoeconomic models suggest that curing a patient saves more than $30,000 in downstream liver disease costs. From a virological perspective, the NS5A inhibitor component reduces the risk of resistance when paired with a nucleotide polymerase inhibitor. Ongoing surveillance studies continue to monitor for rare late‑stage adverse events, and to date the safety record remains reassuring. The WHO’s 2030 elimination target appears increasingly attainable thanks to these therapeutic advances. Nonetheless, achieving universal access will require sustained political will and transparent pricing agreements. Community advocacy groups have successfully pressured manufacturers to adopt tiered pricing structures. In summary, ledipasvir has reshaped both clinical practice and public health strategy, offering a realistic pathway toward a hepatitis‑C‑free world.
Thank you for that comprehensive overview; it really helps put the pieces together and highlights where we can still push for change.