Early Psychosis Intervention: A Simple Guide to Getting Help Fast
If you or someone you know starts showing strange thoughts, hearing voices, or acting oddly, it could be the first signs of psychosis. Acting quickly makes a huge difference – early psychosis intervention (EPI) can stop symptoms from getting worse and improve long‑term outcomes. In this guide we’ll break down why speed matters, what treatments are available, and how to find help without feeling lost.
Why Early Intervention Matters
The brain is still adjusting during the first months of psychotic symptoms. During this window, therapy and medication work best because they can reshape thinking patterns before habits become entrenched. Studies show that people who receive EPI within the first year are less likely to need hospitalization later and often keep jobs or school. In short, a few weeks of action now can save years of struggle.
Another reason timing is key: early symptoms are usually milder. This makes it easier for clinicians to identify what’s going on and choose the right treatment plan. When psychosis is left untreated, stress builds up, social connections fade, and the risk of substance use rises – all of which complicate recovery.
Effective Strategies and What to Expect
EPI isn’t a one‑size‑fits‑all prescription. The most common components include low‑dose antipsychotic medication, specialized cognitive therapy, family education, and coordinated care from a team of mental health professionals. Medication helps calm the brain’s chemistry, while therapy teaches coping skills and reality‑testing techniques that reduce fear.
Family members also get involved. Education sessions show them how to support their loved one without pushing too hard, and they learn signs that signal worsening symptoms. A case manager often coordinates appointments, medication refills, and school or work accommodations, so the person doesn’t have to juggle everything alone.
What does a typical first month look like? You’ll probably start with an intake interview where clinicians ask about your history, current worries, and daily routine. After that comes a quick physical exam and basic lab tests to rule out medical issues. Then the team will set short‑term goals – maybe reducing voice hearing or improving sleep. Follow‑up visits happen every one to two weeks at first, giving the doctor a chance to adjust medication dosage based on how you feel.
Getting started is easier than it sounds. Search online for "early psychosis program" plus your city or ask a primary care doctor for a referral. Many hospitals run dedicated early‑intervention clinics that accept insurance and even offer sliding‑scale fees. If cost is a concern, look for community mental health centers – they often have the same services at lower prices.
Remember, reaching out isn’t a sign of weakness; it’s the smartest move you can make for yourself or someone you care about. Early psychosis intervention gives you tools, support, and a roadmap back to a stable life before symptoms take over.
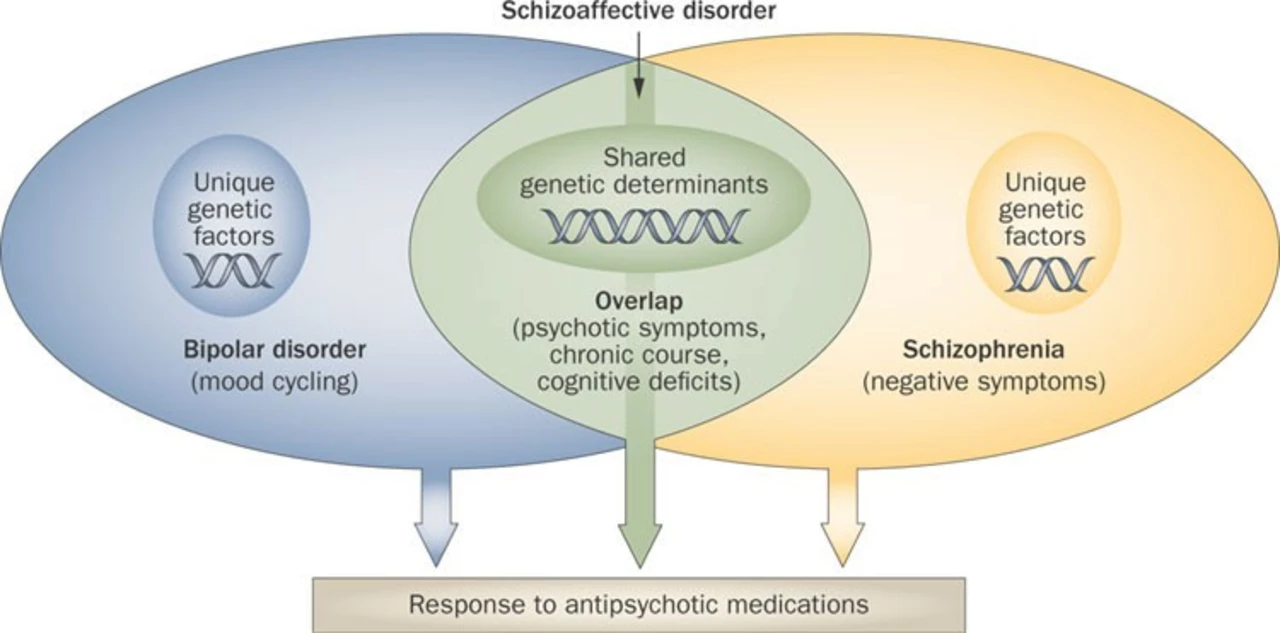
The Role of Ziprasidone in Early Psychosis Intervention
In my latest blog post, I discussed the role of Ziprasidone in early psychosis intervention. Ziprasidone is an atypical antipsychotic medication often used to manage symptoms of schizophrenia and bipolar disorder. Its effectiveness in early psychosis intervention is noteworthy, as it can help reduce the severity of symptoms and improve overall functioning. Additionally, Ziprasidone has a favorable side-effect profile compared to other antipsychotic medications, making it a more desirable option for many patients. Overall, incorporating Ziprasidone into early psychosis intervention strategies has the potential to significantly improve outcomes for individuals experiencing psychotic episodes.