Understanding Early Psychosis Intervention and Ziprasidone
Before diving into the role of ziprasidone in early psychosis intervention, it's essential to understand what early psychosis intervention is and why it's important. Early psychosis intervention is a crucial approach that aims to identify and treat psychotic symptoms as early as possible. This approach has been shown to improve the outcomes for individuals experiencing psychosis and reduce long-term disability.
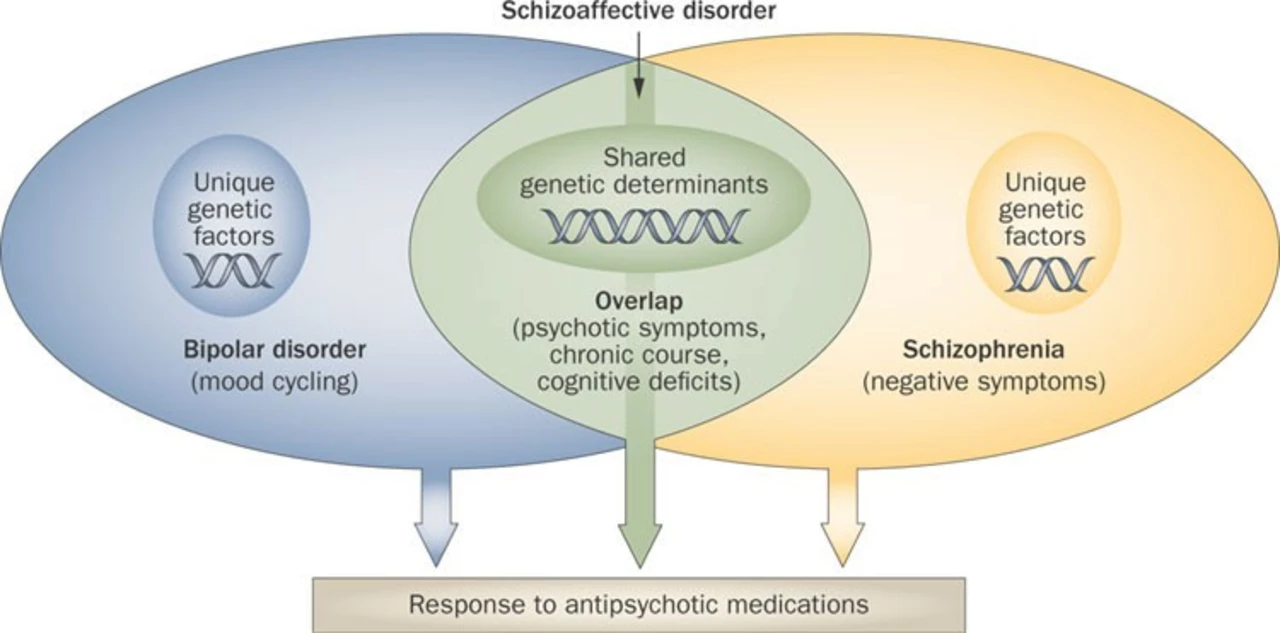
Ziprasidone is an atypical antipsychotic medication commonly prescribed to treat schizophrenia and bipolar disorder. In this article, we will explore how ziprasidone can play a significant role in early psychosis intervention and why it's an essential tool for mental health professionals.
Ziprasidone's Mechanism of Action
Ziprasidone works by targeting specific receptors in the brain, particularly dopamine and serotonin receptors. By blocking these receptors, ziprasidone can help regulate the levels of these neurotransmitters, which are often imbalanced in individuals experiencing psychosis. This helps to alleviate symptoms such as hallucinations, delusions, and disorganized thinking. Additionally, ziprasidone has a relatively low risk of causing extrapyramidal side effects, which are common with other antipsychotic medications. This makes it a more tolerable option for many patients.
Benefits of Early Intervention with Ziprasidone
Research has shown that early intervention with antipsychotic medications, such as ziprasidone, can lead to better long-term outcomes for individuals experiencing psychosis. By starting treatment early, patients are more likely to achieve symptomatic remission and maintain better overall functioning.
Furthermore, early intervention with ziprasidone can prevent the worsening of psychotic symptoms, reduce the risk of relapse, and lessen the likelihood of hospitalization. This not only benefits the individual but also reduces the burden on healthcare systems and the patient's family and support network.
Ziprasidone and Cognitive Functioning
One of the most significant benefits of using ziprasidone in early psychosis intervention is its potential impact on cognitive functioning. Cognitive deficits are common in individuals with schizophrenia and bipolar disorder and can significantly impact daily functioning and quality of life.
Studies have shown that ziprasidone may have a positive effect on cognitive functioning in patients with schizophrenia, potentially improving memory, attention, and executive functioning. This makes it an attractive option for early psychosis intervention, as preserving cognitive function is critical for long-term recovery and life satisfaction.
Reducing the Risk of Metabolic Syndrome with Ziprasidone
Metabolic syndrome is a significant concern for individuals taking antipsychotic medications, as many of these drugs are associated with weight gain, increased blood sugar, and other metabolic complications. However, ziprasidone has a lower risk of causing metabolic syndrome compared to other atypical antipsychotics. This is particularly important for early psychosis intervention, as preventing metabolic complications can improve overall health and long-term outcomes for patients.
Ziprasidone and Sleep Disturbances
Sleep disturbances are common in individuals experiencing psychosis and can exacerbate symptoms and negatively impact overall functioning. Ziprasidone has been shown to improve sleep quality in patients with schizophrenia, which is a crucial component of early psychosis intervention. By promoting better sleep, ziprasidone can help patients achieve greater symptom relief and improve their overall quality of life.
Ziprasidone's Safety and Tolerability
One of the critical factors in selecting an antipsychotic medication for early psychosis intervention is the drug's safety and tolerability. Ziprasidone has a relatively favorable side effect profile compared to other atypical antipsychotics, with a lower risk of causing extrapyramidal symptoms and metabolic complications.
However, it is essential to note that ziprasidone can cause QTc prolongation, which can lead to potentially serious heart complications. As a result, careful monitoring and consideration of potential risk factors are necessary when prescribing ziprasidone for early psychosis intervention.
Psychosocial Interventions and Ziprasidone
While ziprasidone can play a significant role in early psychosis intervention, it's essential to recognize that medication alone is not enough. A comprehensive approach that includes psychosocial interventions, such as cognitive-behavioral therapy, family education, and supported employment, is critical for achieving the best outcomes.
When used in conjunction with these psychosocial interventions, ziprasidone can help patients achieve greater symptom relief, improved functioning, and a better overall quality of life.
Personalizing Treatment with Ziprasidone
It's crucial to remember that each individual experiencing psychosis is unique, and treatment should be tailored to their specific needs. While ziprasidone may be an excellent option for many patients, it's essential to consider factors such as the severity of symptoms, side effect profile, and potential drug interactions when selecting an antipsychotic medication for early psychosis intervention.
By working closely with mental health professionals and considering all available treatment options, individuals experiencing psychosis can receive the best possible care and improve their chances of long-term recovery.
Conclusion
Ziprasidone can play a valuable role in early psychosis intervention by targeting specific neurotransmitter receptors, improving cognitive functioning, and promoting better sleep. Its relatively favorable side effect profile makes it an attractive option for many patients. However, it is important to consider potential risks, such as QTc prolongation, and to combine medication with psychosocial interventions for the best outcomes. By personalizing treatment and working closely with mental health professionals, individuals experiencing psychosis can achieve greater symptom relief, improved functioning, and a better overall quality of life.