Direct-Acting Antivirals: What They Are, How They Work, and Which Ones Matter
When you hear direct-acting antivirals, a class of medications that target specific steps in a virus’s life cycle to stop it from multiplying. Also known as DAAs, they’re the reason hepatitis C is now curable in most cases — no more interferon shots, no more brutal side effects. Before these drugs came along, treating viral infections meant weak, broad-spectrum tools that hurt your body as much as the virus. Direct-acting antivirals changed that by being precise. They don’t just weaken the virus — they shut down its ability to copy itself, one molecular step at a time.
These drugs work by hitting specific viral proteins. For hepatitis C, that means blocking enzymes like NS3/4A protease, NS5A, or NS5B polymerase — the exact tools the virus needs to build new copies. That’s why drugs like sofosbuvir, daclatasvir, and glecaprevir work so well together: each one attacks a different weak point. It’s like cutting three wires on a bomb instead of just one. This precision also means fewer side effects. Unlike older treatments that flooded your whole system, direct-acting antivirals stay focused. And they’re not just for hepatitis C anymore. Researchers are now testing them against hepatitis B, influenza, and even some strains of SARS-CoV-2. They’re becoming the go-to for any virus with a clear, druggable target.
What makes direct-acting antivirals different from older antivirals? Old-school drugs like acyclovir or ribavirin worked by messing with the cell’s DNA or RNA production — which meant they often damaged healthy cells too. DAAs skip that. They only interfere with virus-specific machinery. That’s why cure rates for hepatitis C jumped from 50% to over 95%. It’s not magic — it’s smart design. And because they’re so effective, treatment times dropped from a year to just 8–12 weeks. No more weekly injections. No more constant blood tests just to check if you’re still alive.
You’ll find these drugs in posts about hepatitis C treatments, but you’ll also see them tied to broader topics like drug resistance, combination therapy, and access to care. Some articles dive into how generic versions made these life-saving drugs affordable worldwide. Others warn about what happens when patients skip doses — resistance can creep in, even with DAAs. And while they’re safer than ever, they still need careful use. People with liver disease, kidney problems, or those on other meds need to check for interactions. That’s why you’ll see comparisons between sofosbuvir and velpatasvir, or discussions about which DAA combo works best for genotype 3.
These aren’t just pills. They’re turning once-deadly diseases into manageable ones. And the science behind them is pushing medicine forward — showing that viruses can be beaten with precision, not brute force. What you’ll find below is a collection of real-world guides, comparisons, and updates on how these drugs are being used, improved, and sometimes misused. Whether you’re a patient, a caregiver, or just curious, this isn’t theoretical. It’s about what’s working right now, who it helps, and what to watch out for.
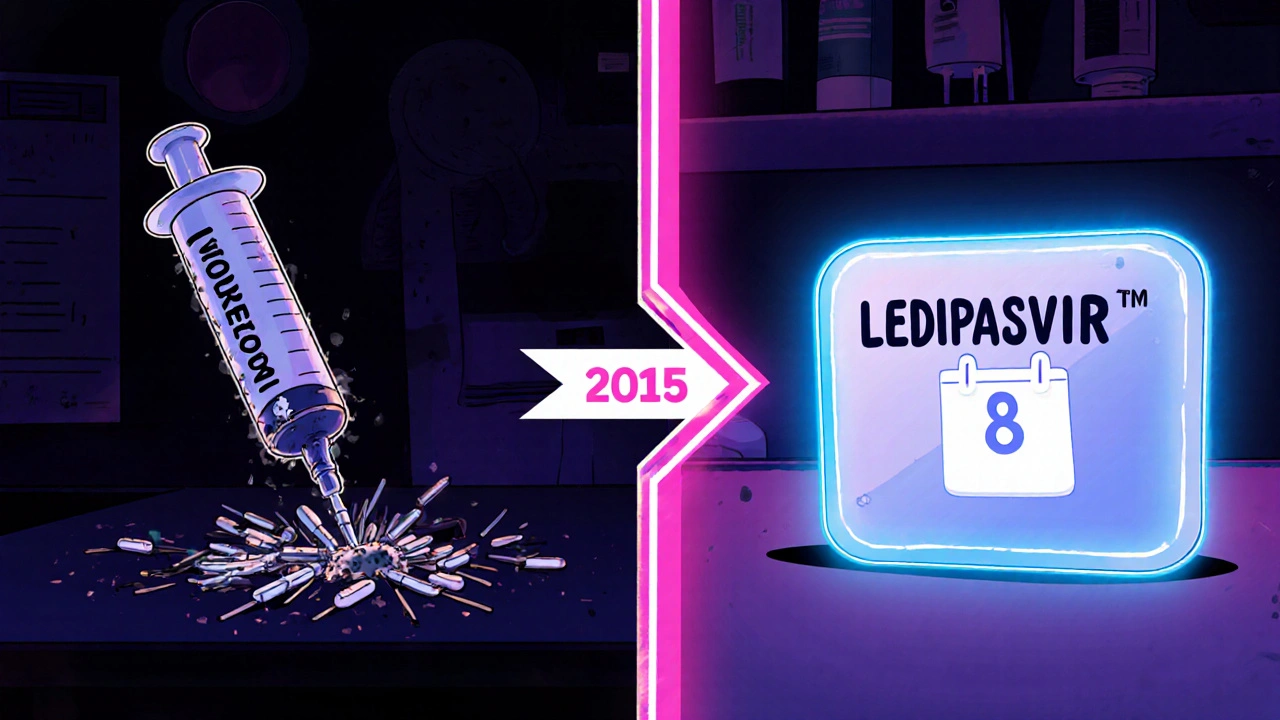
Ledipasvir’s Impact on Global Hepatitis C Treatment
Explore how Ledipasvir transformed hepatitis C therapy worldwide, boosting cure rates, shaping WHO elimination goals, and what challenges and future prospects lie ahead.