Age Considerations in Medication Use: What You Need to Know
When it comes to taking medicine, age considerations, how a person’s age impacts how drugs are absorbed, processed, and eliminated by the body. Also known as pharmacokinetics by age group, it’s not just about how much you take—it’s about how your body changes as you get older or younger. A pill that works fine for a 30-year-old might be too strong for a 70-year-old or too weak for a 5-year-old. Your liver, kidneys, body fat, and even stomach acid all shift over time, and those changes directly affect how medicines behave in your system.
For children, young patients whose organs are still developing and who metabolize drugs differently than adults, dosing isn’t just scaled down from adult amounts. It’s calculated by weight, age, and sometimes even body surface area. Giving a child a crushed adult tablet can be dangerous—many medications aren’t tested for safety in young bodies. That’s why childproofing your home and keeping meds out of reach isn’t just common sense—it’s medical necessity. On the other end of the spectrum, elderly drug metabolism, the slower processing of drugs in older adults due to reduced liver and kidney function means even standard doses can build up to toxic levels. Many seniors take five or more meds daily, and that’s when dangerous interactions happen—like mixing a sleep pill with an antihistamine and triggering anticholinergic overload, which can cause confusion, falls, or even memory loss.
It’s not just about how much you take—it’s about what you’re taking. Some drugs, like certain beta-blockers or statins, carry higher risks for older adults. Others, like SSRIs or GLP-1 agonists, need special monitoring in people with heart conditions that become more common with age. Meanwhile, kids need different treatments for things like rickets or motion sickness, where calcium, vitamin D, or ginger can be safer than pills. Even something as simple as a pain reliever like acetaminophen needs careful dosing in children and older adults to avoid liver damage. The same medicine can save a life or harm it, depending on who’s taking it and when.
Understanding age considerations means recognizing that medicine isn’t one-size-fits-all. It’s why some prescriptions come with warnings like "use with caution in the elderly" or "not for use in children under 12." It’s why your pharmacist asks your age every time you pick up a new script. This collection of articles dives into real-world cases—from how insulin dosing changes for seniors with type 1 diabetes, to why certain antibiotics are avoided in babies, to how cancer drugs are handled differently for older patients. You’ll find clear guidance on what’s safe, what’s risky, and what to ask your doctor when age makes a difference. Whether you’re caring for a child, managing meds as you get older, or just trying to understand why your prescription changed, these posts give you the facts you need to make smarter choices.
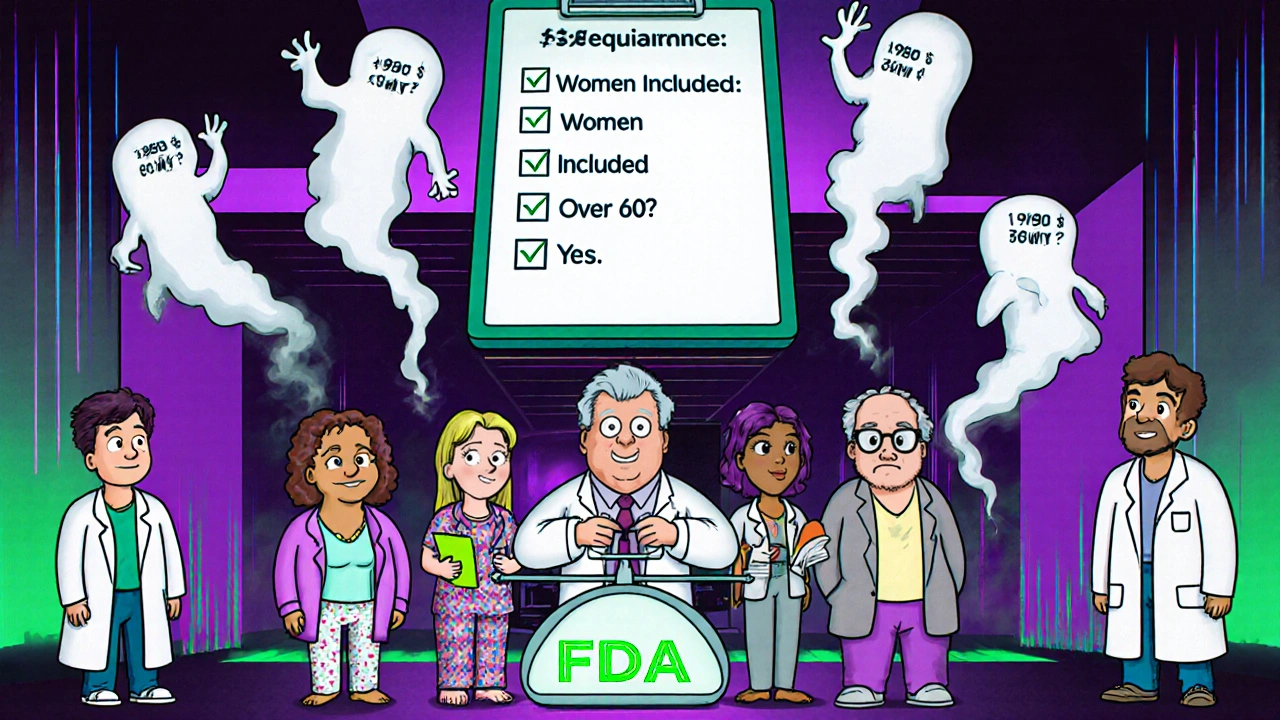
Bioequivalence Studies and the Critical Role of Age and Sex in Study Design
Bioequivalence studies must now include balanced representation of men and women, and older adults, to ensure generic drugs work safely for everyone. Regulatory agencies are updating guidelines to reflect real-world use.