What Are Sedative-Hypnotics, Really?
Sedative-hypnotics are drugs meant to calm your brain and help you sleep. They’re not magic pills - they work by boosting GABA, the brain’s natural calming chemical. But here’s the thing: benzodiazepines and non-benzodiazepines (also called Z-drugs) might sound similar, but they’re not the same. And the risks? They’re bigger than most people realize.
In 2022, over 6 million Americans got prescriptions for non-benzodiazepines like Ambien, Lunesta, or Sonata. Another 3.8 million got benzodiazepines like Xanax, Valium, or Restoril. That’s not just a few people - it’s millions. And yet, the VA’s 2023 guidelines say flat out: It is no longer recommended to take a sedative-hypnotic drug to treat insomnia or anxiety. Why? Because the downsides often outweigh the short-term help.
Benzodiazepines: The Old Guard
Benzodiazepines have been around since the 1950s. Drugs like triazolam, temazepam, and flurazepam bind to multiple GABA-A receptor sites. That means they don’t just help you fall asleep - they also reduce anxiety, relax muscles, and can even stop seizures. That’s why doctors still prescribe them for panic attacks or muscle spasms.
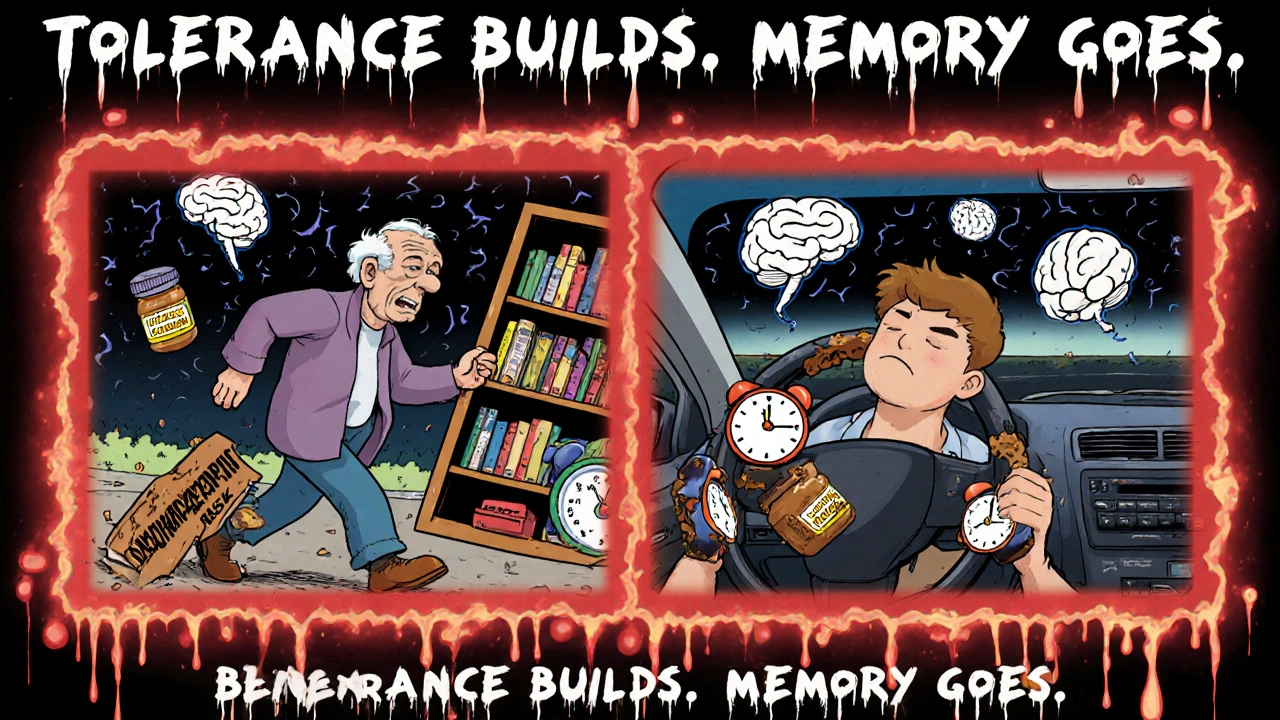
But that broad action is also their biggest flaw. Long-acting ones like flurazepam hang around in your body for days. One study found people on daily flurazepam had considerable impairment of daytime performance - think foggy thinking, slow reactions, trouble concentrating. And it gets worse over time. The drug builds up. Your body doesn’t clear it fast enough. You wake up tired, even if you slept 8 hours.
And then there’s withdrawal. Quitting benzodiazepines cold turkey can trigger seizures, hallucinations, or severe anxiety. One Reddit user who took temazepam for 8 months said quitting led to panic attacks for three weeks straight. That’s not rare. The American Academy of Sleep Medicine says these drugs should only be used for 2-4 weeks. But most people take them longer.
Non-Benzodiazepines: The "Safer" Alternative?
Non-benzodiazepines - zolpidem (Ambien), eszopiclone (Lunesta), zaleplon (Sonata) - were developed in the 1990s as targeted sleep aids. They only bind to one type of GABA receptor (omega-1), which is why they’re marketed as "sleep-specific."
On paper, they look better. Shorter half-lives. Fewer active metabolites. Less daytime grogginess. Zaleplon, for example, lasts just 1-1.5 hours - perfect if you wake up at 3 a.m. and need to fall back asleep fast.
But here’s the catch: they’re not safer in practice. The FDA had to cut zolpidem doses in half for women in 2013 because women were waking up still drowsy, sometimes driving while half-asleep. There were 66% of all sleep-driving incidents between 2005 and 2010 linked to zolpidem. People reported waking up with no memory of the last two hours. One user on Reddit wrote: "I made coffee, brushed my teeth, and drove to the store - and didn’t remember any of it."
And don’t be fooled by "non-addictive" labels. A 2021 meta-analysis found 34% of users had daytime drowsiness severe enough to hurt work performance. And tolerance? It hits fast. In the r/insomnia subreddit, 68% of users said Z-drugs stopped working after two weeks. They upped the dose. Then the side effects got worse.
Side Effects: What No One Tells You
Both classes cause similar side effects: dizziness, dry mouth, nausea, headache. But the scary ones? They’re different.
Benzodiazepines increase your risk of falls and hip fractures by 2.3 times in people over 65. Why? Because they mess with balance, coordination, and reaction time. Even a small dose can make you wobble. A 2012 JAMA study showed older adults on benzodiazepines had higher fracture rates than those on Z-drugs.
Non-benzodiazepines? They’re linked to complex sleep behaviors. Sleepwalking. Sleep eating. Sleep driving. One woman took Lunesta and woke up with her kitchen counter covered in peanut butter and bread - and had no memory of making it. The FDA has issued black box warnings for these behaviors. They’re rare, but when they happen, they’re dangerous.
Both can worsen sleep apnea. If you have untreated sleep apnea - and 20-30% of chronic insomniacs do - these drugs can make breathing worse. That means more oxygen drops, more stress on your heart, and higher risk of high blood pressure or heart attack.
And then there’s memory. A 2024 VA report found a 5-fold higher risk of memory and concentration problems. That’s not just forgetting where you put your keys. It’s forgetting names, appointments, even conversations. And it doesn’t go away right after you stop taking them.
Who Should Avoid These Drugs?
If you’re over 65, avoid both classes. The American Geriatrics Society Beers Criteria lists them as "potentially inappropriate" for older adults. The risk of falls, confusion, and fractures is too high.
If you have liver disease (Child-Pugh Class C), your body can’t break down these drugs properly. Same with severe kidney disease (CrCl under 30 mL/min). Even a normal dose can build up to toxic levels.
And never mix them with alcohol, opioids, or antidepressants. That combo can slow your breathing to a dangerous level - even cause death. WebMD warns that "even the smallest amount of alcohol can interact with sleeping pills." That means one glass of wine? Too much.
What About Long-Term Use?
Here’s the hard truth: neither class works well long-term. Tolerance builds fast. You need more to get the same effect. Then withdrawal hits harder. Studies show 8 weeks of intermittent zolpidem use didn’t improve health or performance at all - even though the study had enough power to detect small changes.
And the long-term data? It’s grim. A 3-year follow-up found people on hypnotics had more doctor visits, more hospital days, and worse quality of life. They reported more physical pain, more depression, more social withdrawal. The drugs didn’t fix insomnia - they made life worse.
The Real Solution: CBT-I
The American Academy of Sleep Medicine says cognitive behavioral therapy for insomnia (CBT-I) is the first-line treatment. Not pills. Not supplements. Therapy.
CBT-I teaches you how to fix the thoughts and habits that keep you awake. It includes sleep restriction, stimulus control, and relaxation training. Studies show it works better than pills - and the effects last. After stopping CBT-I, people stay asleep. After stopping pills? Insomnia comes back, often worse.
And it’s accessible. Many insurance plans cover it. Online programs like Sleepio and CBT-I Coach have been proven effective. No pills. No side effects. No withdrawal.
What If You’re Already on These Drugs?
If you’ve been taking them for months or years, don’t quit cold turkey. That’s dangerous. Talk to your doctor about tapering.
Benzodiazepines usually need a slow taper - reduce by 10% every 1-2 weeks. Some people take months to get off. Z-drugs can be tapered faster - often over 2-4 weeks. But even then, you might feel anxious, restless, or have rebound insomnia. That’s normal. It doesn’t mean you failed. It means your body adjusted to the drug.
Keep a sleep diary. Note when you take the pill, how you feel the next day, if you dream, if you wake up confused. Bring it to your doctor. They need to see the real picture.
The Bottom Line
Benzodiazepines and non-benzodiazepines aren’t bad drugs. They can help in a crisis - a night after a death, a week after surgery, a few days during extreme stress. But they’re not for long-term sleep problems.
The risks - memory loss, falls, addiction, sleepwalking, worsened apnea - are real. And they’re growing as our population ages. The CDC data shows benzodiazepine prescriptions have dropped since 2013, but Z-drugs have crept up. That’s not progress. It’s a shift in branding, not safety.
If you’re struggling with sleep, ask your doctor about CBT-I. It’s not flashy. It takes work. But it’s the only treatment that actually fixes insomnia - without putting your life at risk.

