Immunosuppressant Selection Guide
Patient Selection Tool
Answer these questions to determine the most appropriate immunosuppressant for your patient.
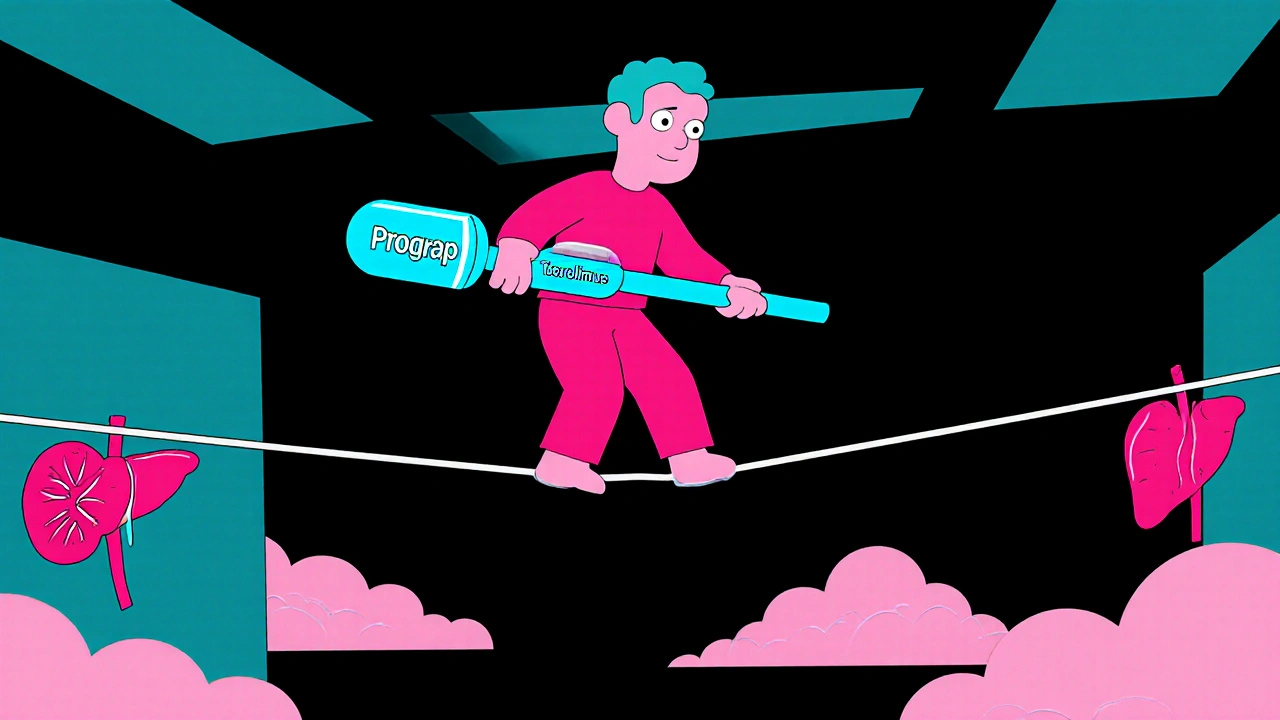
When a patient faces organ transplantation, the choice of immunosuppressant can feel like walking a tightrope. One drug that shows up on most doctors’ lists is Prograf (Tacrolimus), a calcineurin inhibitor that blocks T‑cell activation. Prograf has become a go‑to for many because it balances potency with a relatively manageable safety profile. But it isn’t the only player on the field. Below we compare Prograf with the most common alternatives, so you can see where each drug shines and where it falters.
What Is Prograf (Tacrolimus) and How Does It Work?
Prograf (Tacrolimus) belongs to the calcineurin‑inhibitor class. It binds to the immunophilin FKBP‑12, forming a complex that stops calcineurin from activating the nuclear factor of activated T‑cells (NFAT). The result? T‑cells stay idle, and the immune system doesn’t launch a full‑blown attack on a new organ.
Key Indications for Prograf
Prograf is approved for:
- Kidney transplantation
- Liver transplantation
- Heart transplantation
- Skin conditions like severe atopic dermatitis (off‑label)
Because it works quickly and has a predictable blood‑level profile, transplant surgeons often start patients on Prograf right after surgery.
Typical Dosing and Monitoring
Dosing is individualized. Most adults start with 0.1 mg/kg twice daily, then adjust based on trough levels (usually 5-15 ng/mL for kidney transplants). Blood‑level monitoring is essential; too low and you risk rejection, too high and you invite nephrotoxicity.
Common Side Effects to Watch
Even with careful monitoring, patients can experience:
- Nephrotoxicity
- Neurotoxicity (tremor, headaches)
- Hyperglycemia
- Hypertension
- Increased infection risk
Most side effects are dose‑dependent, which is why therapeutic drug monitoring (TDM) is a non‑negotiable part of the regimen.
Alternative Immunosuppressants
Below are the main alternatives that clinicians consider when Prograf isn’t a perfect fit.
Cyclosporine
Another calcineurin inhibitor, cyclosporine binds to cyclophilin instead of FKBP‑12. It’s been around longer than Tacrolimus and is still used for liver and heart transplants. The drug has a narrower therapeutic window and tends to cause more gum hyperplasia and hirsutism.
Sirolimus
Sirolimus (also called rapamycin) is an mTOR inhibitor, not a calcineurin blocker. It prevents T‑cell proliferation rather than activation. Because it spares the kidneys, Sirolimus is a favorite when clinicians want to avoid Tacrolimus‑related nephrotoxicity. However, it can delay wound healing and cause hyperlipidemia.
Mycophenolate mofetil
Mycophenolate interferes with guanine nucleotide synthesis, curbing B‑ and T‑cell proliferation. It’s typically combined with a calcineurin inhibitor but can serve as a sole agent in low‑risk patients. GI upset and bone marrow suppression are its biggest drawbacks.
Azathioprine
Azathioprine is a purine analog that dampens lymphocyte activity. It’s older, cheaper, and often used in maintenance therapy after the initial high‑intensity phase. Its slow onset makes it unsuitable for early post‑transplant periods, and liver toxicity can be a concern.
Everolimus
Everolimus is a newer mTOR inhibitor, similar to Sirolimus but with a shorter half‑life. It’s approved for kidney and liver transplants and can be paired with reduced‑dose Tacrolimus to limit nephrotoxicity. The trade‑off is an increased risk of mouth ulcers and proteinuria.
Belatacept
Belatacept is a costimulation blocker that binds CD80/CD86, preventing T‑cell activation. It’s administered intravenously once a month and was designed to replace calcineurin inhibitors in kidney transplantation. While it spares the kidneys, the infusion schedule and higher infection risk keep it from being first‑line.
Side‑by‑Side Comparison Table
| Drug | Class | Primary Mechanism | Typical Indications | Key Side Effects | Monitoring Needed |
|---|---|---|---|---|---|
| Prograf (Tacrolimus) | Calcineurin inhibitor | Blocks calcineurin → NFAT | Kidney, liver, heart transplants | Nephrotoxicity, neurotoxicity, hyperglycemia | Trough blood levels 5‑15 ng/mL |
| Cyclosporine | Calcineurin inhibitor | Blocks calcineurin via cyclophilin | Liver, heart transplants | Nephrotoxicity, gum hyperplasia, hirsutism | Trough levels 150‑300 ng/mL |
| Sirolimus | mTOR inhibitor | Inhibits mTOR → cell cycle arrest | Kidney, liver transplants (often combo) | Delayed wound healing, hyperlipidemia | Therapeutic range 5‑15 ng/mL |
| Mycophenolate mofetil | Antimetabolite | Inhibits IMP dehydrogenase | Maintenance therapy, combo regimens | GI upset, leukopenia | Drug‑level monitoring not routine |
| Azathioprine | Purine analog | Inhibits DNA synthesis in lymphocytes | Long‑term maintenance, steroid‑sparing | Liver toxicity, bone‑marrow suppression | Periodic CBC, liver function tests |
| Everolimus | mTOR inhibitor | Blocks mTOR signaling | Kidney, liver transplants (low‑dose Tac combo) | Mouth ulcers, proteinuria | Target trough 3‑8 ng/mL |
| Belatacept | Costimulation blocker | Prevents CD80/86 interaction | Kidney transplantation (alternative to CNI) | Infections, PTLD risk | Monthly IV infusion, no routine blood level |

How to Choose the Right Immunosuppressant
There’s no one‑size‑fits‑all answer. Here’s a quick decision framework:
- Kidney protection needed? If the patient already shows signs of reduced renal function, lean toward mTOR inhibitors (Sirolimus or Everolimus) or a reduced‑dose Tacrolimus.
- Risk of infection? Belatacept and high‑dose Tacrolimus raise infection risk; Mycophenolate or Azathioprine may be safer in low‑immunity settings.
- Wound‑healing concerns? Avoid Sirolimus/Everolimus in the first 4‑6 weeks post‑surgery.
- Cost and access? Generic Cyclosporine and Azathioprine are cheaper, but may need more lab work.
- Patient preference for route? Belatacept requires monthly IV; all others are oral.
Discuss these points with the transplant team, pharmacists, and the patient. A shared decision often leads to better adherence.
Practical Tips for Managing Tacrolimus Therapy
- Always take the drug at the same times each day-consistency reduces trough swings.
- Avoid grapefruit juice; it can raise Tacrolimus levels dramatically.
- Inform your doctor before adding new antibiotics or antifungals; many interact via CYP3A4.
- Monitor kidney function (creatinine, eGFR) at least monthly for the first six months.
- Report new tremors, headaches, or visual changes immediately-they may signal neurotoxicity.
Frequently Asked Questions
Is Tacrolimus stronger than Cyclosporine?
Generally, yes. Tacrolimus requires lower blood concentrations to achieve the same immunosuppressive effect, which is why many clinicians prefer it for high‑risk transplants.
Can I switch from Tacrolimus to an mTOR inhibitor?
Switching is possible, but it must be done gradually under close monitoring. The transplant team usually reduces Tacrolimus over 1‑2 weeks while titrating the mTOR drug to target levels.
What food interactions should I watch for?
Avoid grapefruit and pomelo, as they inhibit CYP3A4 and can push Tacrolimus levels too high. High‑fat meals can also affect absorption, so try to take the medication with a consistent light snack.
How often should blood levels be checked?
Initially, twice a week for the first month, then weekly for the next month, and eventually every 2‑4 weeks once stable. Adjustments depend on kidney function and any new meds.
Is Belatacept a good option for patients with kidney disease?
Belatacept can protect kidney function because it avoids calcineurin‑related nephrotoxicity. However, its monthly IV requirement and higher infection risk make it suitable mainly for patients who can tolerate frequent clinic visits.
I’ve read every single line of the Tacrolimus monograph and still feel like the drug is a double‑edged sword.
Sure, it’s hailed as the gold standard for kidney and liver transplants, but the side‑effect profile reads like a horror novel.
Nephrotoxicity can silently creep in while you’re busy adjusting trough levels, and before you know it the patient’s own kidneys are begging for a break.
Add neurotoxicity-tremors, headaches, occasional visual disturbances-and you’ve got a cocktail that can turn a hopeful transplant recipient into a walking nightmare.
And let’s not forget the metabolic havoc: hyperglycemia, hypertension, and the insidious weight gain that follows a high‑dose regimen.
The monitoring nightmare is another beast entirely; you’re forced to sit in a lab chair twice a day, praying the levels stay in the narrow therapeutic window.
Meanwhile, the alternatives each parade their own quirks, like cyclosporine’s gum hyperplasia that makes you look like a 90‑year‑old beaver.
Sirolimus spares the kidneys, but then you have delayed wound healing that can turn a routine incision into a chronic ulcer.
Mycophenolate’s GI upset feels like a daily gamble with nausea, while azathioprine’s liver toxicity is the silent assassin you only discover after months of therapy.
Everolimus promises a shorter half‑life, yet the mouth ulcers it triggers can make eating a painful chore.
Belatacept’s IV schedule sounds convenient on paper, until the infusion center becomes a monthly prison and the infection risk spikes like a broken dam.
In practice, the choice is rarely about “better” or “worse” and more about which devil you’re willing to dance with for a few precious years.
If your patient already shows signs of renal impairment, the temptation to skip Tacrolimus for an mTOR inhibitor is strong, but you risk poor wound healing and dyslipidemia.
Conversely, a robust patient with a stable kidney might tolerate Tacrolimus’s nephrotoxic potential if the immunosuppression keeps rejection at bay.
Bottom line: there is no universal champion, only a precarious balance of risks that must be individualized for every transplant case.
Oh, so you think Tacrolimus is the holy grail? Think again, dear clinicians.
This calcineurin inhibitor is just a glorified neuro‑toxic party animal that loves to mess with your blood sugar.
And don’t even get me started on cyclosporine’s gum hyperplasia – it’s like a dental horror show.
Sure, Sirolimus spares the kidneys, but you’ll be waiting forever for a wound to close.
In short, every drug on this list has a hidden agenda, and pharma loves us to believe otherwise.
While drama abounds, the moral imperative remains: we must protect the graft above all else.
The evidence still shows Tacrolimus reduces acute rejection more effectively than cyclosporine in most trials.
Yes, the side‑effects are real, but they are manageable with diligent monitoring and patient education.
Throwing away a drug just because it’s “dramatic” ignores the hard‑won data from decades of transplant practice.
Let’s not sacrifice efficacy for a false sense of safety; balance is key.
In my view, individualized protocols that incorporate TDM are the ethical path forward.
Great rundown, everyone.
Just a heads‑up: patients often forget to avoid grapefruit juice, which can really spike Tac levels.
Also, keeping a consistent dosing schedule helps flatten those trough swings.
Overall, a team‑approach with pharmacists makes the whole thing smoother.
Listen, the whole immunosuppressive armory is a product of Big Pharma’s profit machine.
They push Tacrolimus because it’s a patented cash cow, not because it’s the safest choice.
Ever notice how the newer mTOR inhibitors are marketed as “kidney‑friendly” just before patents expire?
And the monthly IV belatacept? Perfect for clinics to rack up infusion fees.
Don’t be fooled – the real cure is careful patient selection, not a pharmaceutical hype cycle.
Valid concerns, but let’s keep perspective.
When counseling patients, I emphasize that each agent has a risk‑benefit profile that can be matched to their clinical picture.
For example, a patient with pre‑existing renal dysfunction might benefit from an mTOR‑based regimen with reduced Tac dose.
Monitoring protocols have improved, and drug‑interaction tools help avoid the grapefruit trap you mentioned.
Ultimately, shared decision‑making empowers patients and mitigates the profit‑driven narrative.
Tacrolimus is a tightrope; walk carefully.
Thanks for the thorough breakdown.
Pretty helpful for anyone trying to navigate this maze.
While the article is comprehensive, a few clarifications are in order: the trough levels for cyclosporine are expressed in ng/mL, not mg/L; the hyperlipidemia risk associated with Sirolimus often necessitates statin therapy, which introduces additional drug‑interaction considerations; Belatacept’s infection risk is predominantly viral, especially EBV‑related PTLD; the mTOR inhibitors’ delayed wound healing typically manifests within the first 4‑6 weeks post‑operatively; finally, patient adherence to oral regimens can be impacted by the pill burden, which the table does not address.
Immunosuppression is the art of controlled surrender, a paradox where we deliberately weaken our defenses to preserve life.
It’s a reminder that medicine often walks the line between cure and compromise.
The practical tips are spot‑on; consistent timing and awareness of food interactions make a huge difference.
I’ll definitely pass this along to my older aunt who’s awaiting a kidney transplant.
Let’s dissect the table a bit more.
First, the classification column could benefit from specifying the exact molecular target, e.g., FKBP‑12 for Tacrolimus, cyclophilin for cyclosporine.
Second, the “Key Side Effects” for Mycophenolate omit the risk of opportunistic infections like CMV, which is clinically relevant.
Third, under Azathioprine, the liver toxicity mention should be quantified; transaminases can rise up to three times baseline in 10‑15% of patients.
Fourth, the monitoring column for Everolimus should note that therapeutic drug monitoring is recommended especially when combined with CYP3A4 inhibitors.
Fifth, the Belatacept row could indicate that pre‑transplant EBV serostatus is a prerequisite to mitigate PTLD risk.
Lastly, a footnote about drug‑interaction potential with common antibiotics (e.g., clarithromycin) would round out the practical guidance.
Your exhaustive list still omits the human cost of relentless monitoring and endless lab draws.
Patients often feel like lab rats, their lives reduced to numbers on a screen.
Even with perfect troughs, the psychological toll of constant vigilance can be crushing.
We need to remember that medicine is as much about compassion as it is about chemistry.
Let’s not lose sight of the person behind the protocol.