When a patient walks into the pharmacy with a prescription for a biologic drug like Neulasta or Humira, they’re not just getting a pill - they’re getting a complex, high-cost treatment that can cost thousands per month. That’s where pharmacists step in. Not as silent fillers of prescriptions, but as active guides through one of the biggest shifts in modern medicine: the rise of biosimilars.
Biosimilars aren’t generics. That’s the first thing every pharmacist needs to make crystal clear - to patients, to doctors, and to themselves. Generics are exact chemical copies of small-molecule drugs. Think of them like a photocopy of a handwritten note: same words, same ink, same paper. Biosimilars? They’re more like a hand-drawn replica of a Picasso. The image looks nearly identical, but the brushstrokes, the texture, the way it was made - those details vary because they come from living cells, not a chemistry lab. The FDA says they’re “highly similar” with no clinically meaningful differences in safety or effectiveness. But that doesn’t mean patients believe it. And that’s where counseling becomes critical.
Why Pharmacists Are the Key to Biosimilar Adoption
Biologics make up only 2% of all prescriptions in the U.S., yet they account for nearly half of all prescription drug spending. That’s a massive financial burden - on insurers, on patients, on the whole system. Biosimilars can cut those costs by 15% to 35%, sometimes more. But adoption has been slow. Why? Because doctors are hesitant. Patients are scared. And laws are all over the map.
Enter the pharmacist. A 2022 study in the Journal of Managed Care & Specialty Pharmacy found that 87.3% of pharmacists recommended biosimilars to patients - compared to just 62.1% of physicians. Why? Because pharmacists are the ones who see the whole picture: the cost, the supply chain, the patient’s history, the insurance formulary, and the real-world data on switching.
At the US Oncology Network, they turned things around by shifting substitution from physician-driven to pharmacy-driven. Before, every switch required a phone call, a note, a delay. After, pharmacists were authorized to swap out the brand-name drug for its biosimilar - as long as the prescriber had signed off on a standing policy. The result? Within months, adoption of the pegfilgrastim biosimilar jumped from almost zero to over 80%. No more daily interruptions for doctors. No more delays for patients. Just a smoother, smarter system.
Interchangeable vs. Non-Interchangeable: What’s the Difference?
Not all biosimilars are created equal. The FDA has a special designation: interchangeable. This means the biosimilar can be swapped in without the prescriber’s input - just like a generic. But here’s the catch: as of late 2023, only a handful of biosimilars have this status. Most still require the prescriber to say “dispense as written” or “allow substitution.”
That’s where state laws come in. Forty-eight states have passed some kind of biosimilar substitution law. But they’re messy. Some require the pharmacist to notify the prescriber within 24 hours. Some require patient consent in writing. Others let pharmacists substitute automatically - but only if the drug is labeled interchangeable. If you’re a pharmacist in Texas, your rules are different than in New York. And if you’re in a clinic that doesn’t track batch numbers? You’re not just risking patient safety - you’re risking legal liability.
Traceability isn’t optional anymore. Every biosimilar dispensed must include the product name, manufacturer, and batch number - on the label, in the record, and often handed to the patient on a paper slip. Why? Because if someone has a bad reaction, you need to know exactly which version they got. This isn’t just paperwork. It’s pharmacovigilance. And pharmacists are the frontline.
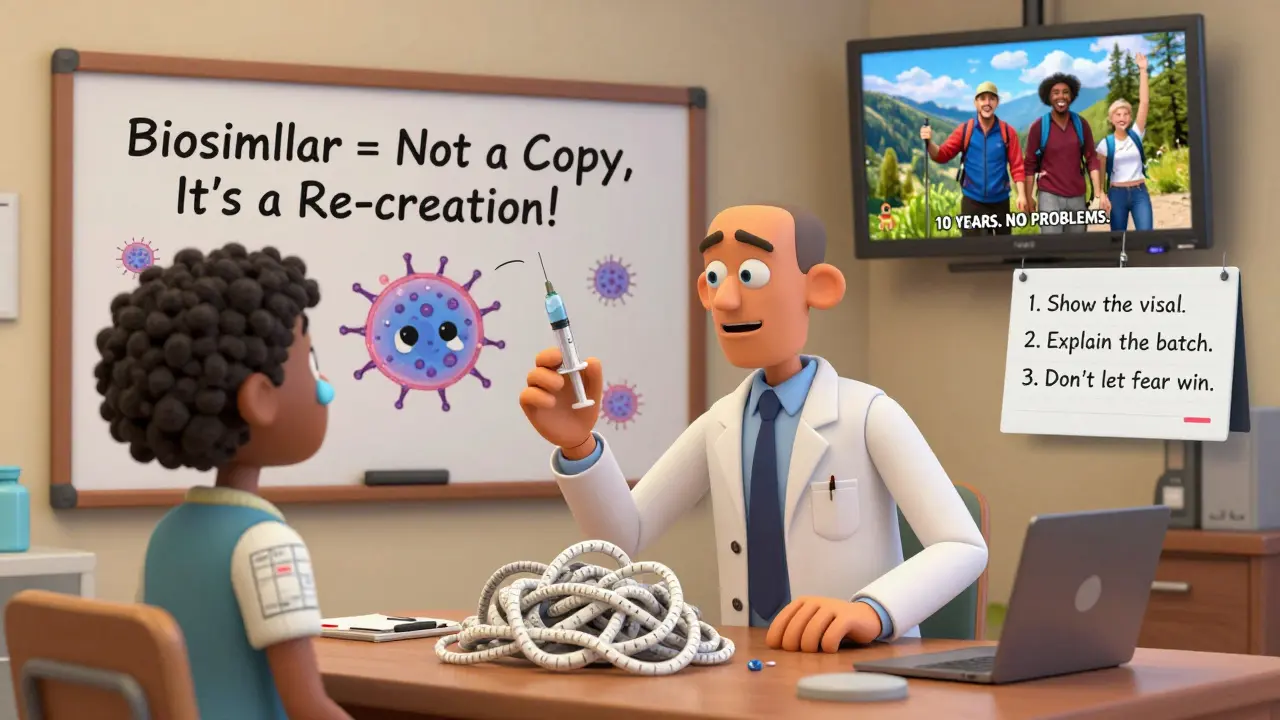
Counseling Patients: Breaking the Myths
One pharmacist in Manchester told me: “I had a patient cry because she thought switching meant her cancer treatment was being ‘downgraded.’” That’s the fear we’re fighting.
Patients hear “biosimilar” and think “cheap copy.” They worry about side effects. They fear their disease won’t be controlled. Some even think switching means they’re being treated like a guinea pig.
But the science doesn’t back that up. Studies show switching from a reference biologic to a biosimilar - even multiple times - doesn’t increase risk. The FDA approved biosimilars based on over 100 clinical trials. Real-world data from Europe, where biosimilars have been used for over a decade, shows no drop in effectiveness or safety.
So how do you talk to patients? Start simple:
- “This isn’t a generic. It’s a different kind of copy - made from living cells, not chemicals.”
- “The FDA says it works just like the original. No meaningful differences.”
- “Thousands of people have switched. No new side effects. No loss of control.”
- “It’s the same treatment. Just less expensive. That means more people can get it.”
And don’t ignore the physical changes. If the pill size, color, or injector design changes, patients notice. And that’s a red flag. Research shows patients are 21% more likely to stop taking their medication if it looks different. So show them the new package. Point out the batch number. Let them hold it. Let them ask. That’s not extra work - that’s trust-building.
What Pharmacists Need to Know - And Do
Being a pharmacist in the biosimilar era isn’t just about counting pills anymore. It’s about being a bridge - between science and fear, between policy and practice, between cost and care.
Here’s what you need to do:
- Know your state’s law. Is substitution automatic? Is consent required? Is notification mandatory? Don’t guess. Check your state board’s website monthly - laws change.
- Track every batch. Use your pharmacy system to record the exact product and lot number dispensed. This isn’t just for audits - it’s for patient safety.
- Educate your team. Nurses, medical assistants, financial counselors - they all get questions. Train them on the basics. A 2022 survey found that 79% of pharmacists wanted more education on billing and reimbursement. If you’re not trained, how can you help?
- Partner with prescribers. Don’t wait for them to complain. Send them a one-pager: “Here’s how we’re handling biosimilar substitution. Here’s the data. Here’s how we’re protecting your patients.”
- Document everything. If you substitute, write it down. If you don’t, write why. If the patient refuses, document that too. Paper trails save jobs.

The Bigger Picture: Why This Matters
Biologics are the future. Cancer drugs. Autoimmune treatments. Rare disease therapies. They’re complex. They’re expensive. And they’re here to stay.
Biosimilars are the only tool we have to make them affordable. Without them, millions of patients will be priced out. Insurance companies will keep raising premiums. Hospitals will cut services.
Pharmacists are the only professionals who see the full chain: from the manufacturer’s lab, to the warehouse, to the patient’s hand. We’re the ones who can explain the science. We’re the ones who can enforce the rules. We’re the ones who can turn fear into trust.
The data is clear: when pharmacists lead, adoption soars. When we stay silent, patients suffer - not from the disease, but from the cost of not acting.
What’s Next?
The FDA is considering dropping the separate “interchangeable” label altogether. That could change everything. If every biosimilar is treated like it can be swapped automatically, pharmacists will have even more power - and more responsibility.
One thing won’t change: the need for skilled, informed, compassionate pharmacists who don’t just fill prescriptions - they change outcomes.
Can a pharmacist substitute a biosimilar without the doctor’s permission?
Only if the biosimilar is FDA-designated as "interchangeable" AND your state’s law allows automatic substitution. Even then, the prescriber can write "dispense as written" on the prescription, which legally blocks substitution. Pharmacists must check both the drug’s status and the state’s regulations before making a switch.
Are biosimilars as safe as the original biologic drugs?
Yes. The FDA requires biosimilars to undergo rigorous testing to prove they have no clinically meaningful differences in safety, purity, or potency compared to the reference product. Real-world data from Europe and the U.S. - including over 100 clinical trials - confirms this. Switching between a biologic and its biosimilar, even multiple times, has not been linked to increased risks.
Why do some patients stop taking their biosimilar?
The most common reason is a change in appearance - the pill or injector looks different. Studies show patients are 21% more likely to discontinue treatment if the medication looks unfamiliar. Other reasons include misinformation (thinking it’s a "cheap copy") or lack of clear counseling. Pharmacists who take time to explain the science and show the patient the product details can reduce this risk significantly.
Do pharmacists need special training to handle biosimilars?
Yes. Unlike generics, biosimilars require understanding of complex manufacturing, regulatory pathways, state laws, and pharmacovigilance requirements. Many pharmacists report gaps in their knowledge. Continuing education on biosimilars - especially on interchangeability, billing, and patient counseling - is essential. Over 79% of pharmacists surveyed in 2022 requested more training in this area.
What’s the biggest barrier to biosimilar adoption?
It’s not cost - it’s trust. While biosimilars can save 15-35%, prescriber hesitation and patient fear are the main blockers. Many doctors don’t fully understand the science. Many patients fear switching. Pharmacists who actively educate both groups - using clear, evidence-based language - are the most effective at overcoming this barrier.

