The U.S. Food and Drug Administration (FDA) doesn’t just approve drugs and medical devices - it keeps watching them long after they hit the market. That’s where MedWatch comes in. It’s not a fancy app or a high-tech dashboard. It’s a quiet, behind-the-scenes system that collects reports from doctors, patients, and manufacturers when something goes wrong. Think of it as the nation’s early warning system for dangerous side effects, faulty implants, or unexpected reactions to medications. Since 1993, MedWatch has been the backbone of the FDA’s post-market safety monitoring. And while most people have never heard of it, millions of reports have flowed through it - and some of those reports have saved lives.
What Exactly Is MedWatch?
MedWatch, officially called the FDA Safety Information and Adverse Event Reporting Program, is the FDA’s main channel for gathering reports about problems with FDA-regulated products. That includes prescription drugs, over-the-counter medicines, vaccines, medical devices like pacemakers and insulin pumps, even cosmetics and hemp-based products. It’s not a law enforcement tool. It’s a reporting and information hub. The system does two things: it lets people report bad experiences, and it sends out alerts when new risks are found.
There are two types of reports that feed into MedWatch. One is voluntary. Anyone - a patient, a nurse, a pharmacist, or even a family member - can file a report if they notice something unusual. The other is mandatory. Companies that make these products are legally required to report serious problems they become aware of. If a manufacturer learns their device caused a death or serious injury, they have to notify the FDA within 30 days. For life-threatening situations, it’s just five workdays.
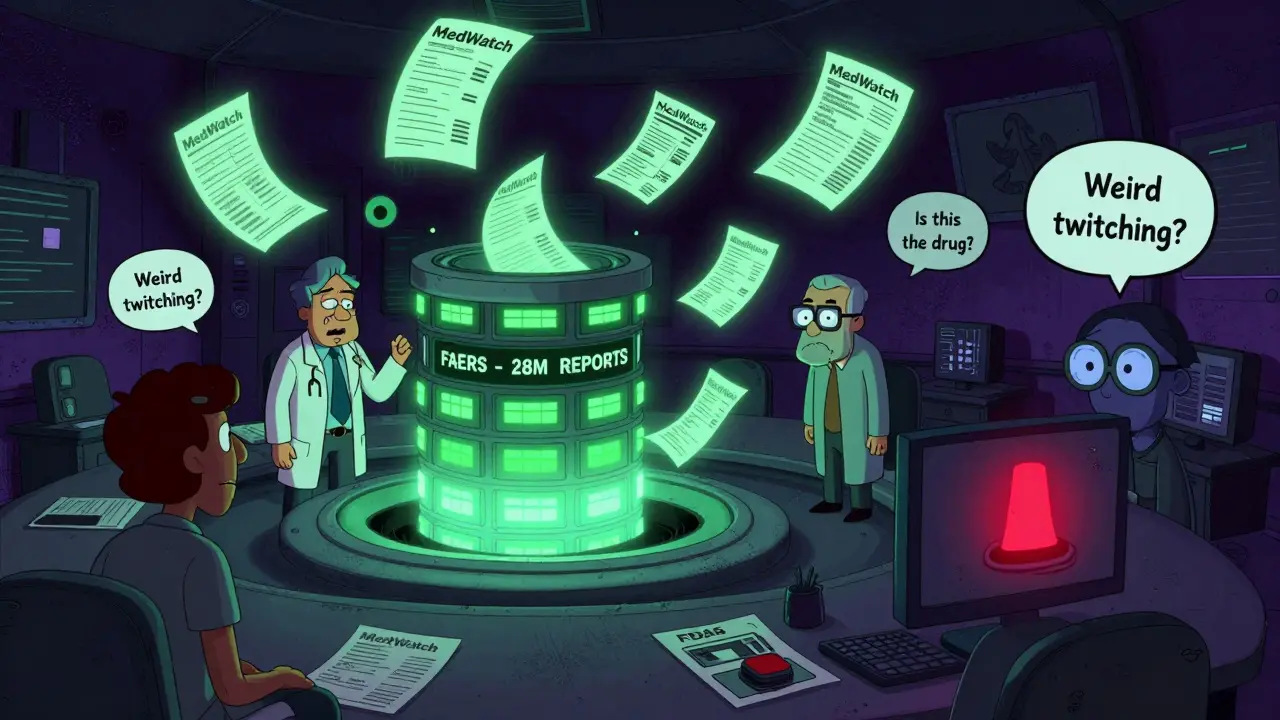
All these reports go into a massive database called the FDA Adverse Event Reporting System (FAERS). As of late 2023, FAERS held over 28 million reports. That’s not just data - it’s a trail of real-world experiences. And from that trail, the FDA looks for patterns. A single report might be ignored. But if 50 people report the same rare reaction to a new blood thinner? That’s a signal. And signals trigger investigations.
How Reports Are Made - And Why Most Never Get Filed
Filing a MedWatch report isn’t hard. The FDA’s online form asks for basic details: patient age and sex, the product name, what happened, when it happened, and what happened afterward. The agency even gives you a checklist: include the patient’s medical history, other drugs they were taking, lab results if available, and how the problem was treated.
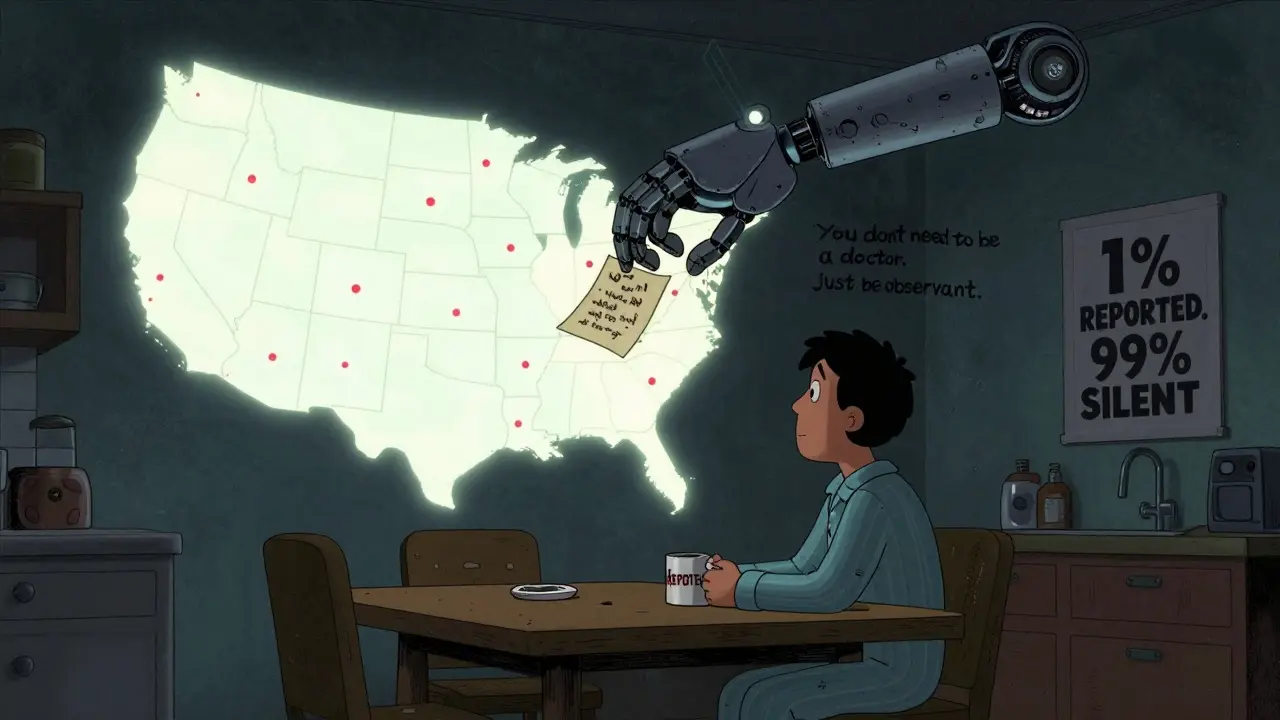
But here’s the problem: most problems never get reported. Studies estimate that only 1% to 10% of adverse events ever make it to MedWatch. Why? Because reporting takes time. A 2021 study by the American Medical Association found that healthcare professionals spend 15 to 20 minutes filling out a single report. For busy doctors, that’s a lot of paperwork. Even with electronic health record integrations - which cut the time to 8 to 12 minutes for some - many still skip it.
Patients face even bigger hurdles. A 2022 survey by the National Consumers League found that 68% of people who tried to report a problem got stuck because they didn’t know how to describe symptoms using medical terms. One woman reported her husband’s “weird twitching” after taking a new medication. The system flagged it as “insufficient detail.” She gave up. That report never made it into the system.
And then there’s the question of causality. You don’t have to prove the drug caused the problem. You just have to report it. The FDA doesn’t need proof - they need clues. But many people think, “It might just be a coincidence,” and stay silent.
Real Cases Where MedWatch Made a Difference
MedWatch isn’t theoretical. It has directly influenced FDA actions. In 2021, the agency recalled Allergan’s BIOCELL textured breast implants after MedWatch reports showed a pattern of rare immune system cancers. The signal was spotted in November. By December, the FDA issued a safety alert. By January, the company was ordered to pull the product. That happened in just 45 days - because of reports from patients and doctors.
Another example: Dr. Sarah Johnson, an oncologist at MD Anderson, submitted a report in 2019 about three patients who developed severe immune reactions after receiving Keytruda, a cancer drug. The reaction was rare, and no one else had reported it. But her detailed report - including lab values and timing - helped the FDA confirm the pattern. Within 90 days, the drug’s label was updated to warn doctors about the risk.
These aren’t outliers. Between 2015 and 2020, MedWatch reports contributed to 37% of all FDA safety communications, according to former FDA Commissioner Dr. Janet Woodcock. That’s nearly four out of every 10 warnings you’ve seen on drug labels or news alerts - traced back to someone taking the time to report.

Who Reports - And Who Doesn’t
Not everyone reports equally. In 2022, 42% of MedWatch reports came from patients and caregivers. That’s higher than in most other countries. The U.S. system is unique because it’s open to the public. In Europe, reports mostly come from healthcare providers. In Canada, it’s mostly professionals too.
But industry reports dominate the numbers. Pharmaceutical companies account for 78% of all submissions. Medical devices make up 15%. The rest? Biologics and other products. Why? Because manufacturers are legally required to report. Patients aren’t. And that creates a blind spot.
When a drug causes mild nausea in 10% of users, manufacturers report it - because it’s common. But when a rare but deadly reaction happens in one in 10,000, it’s often the patient who notices first. And if that patient doesn’t report? The FDA might never know.
The Future of MedWatch - And the Big Challenges
The FDA is trying to fix the system. In September 2023, they launched MedWatch Direct, a new API that lets electronic health records automatically send reports. Epic, Cerner, and other major health systems are testing it. If it works, reporting could become as easy as clicking “submit” after a patient visit.
By 2024, the FDA plans to use artificial intelligence to scan clinical notes for signs of adverse events. Instead of waiting for someone to file a report, AI might pull the warning right out of a doctor’s handwritten note. That could increase reporting rates by 25%.
But even with better tech, the core problem remains: underreporting. The Government Accountability Office called it a “critical gap.” Dr. Peter Lurie of the Center for Science in the Public Interest put it bluntly: “No amount of AI can fix a system where most problems go unreported.”
The FDA has only 120 full-time staff analyzing over 1.2 million reports each year. That’s about 10,000 reports per person. No human can dig through that much data deeply. They rely on algorithms to flag the most urgent signals. But algorithms can miss subtle patterns - especially if the data is sparse.
What You Can Do
If you’ve had a bad reaction to a medication or device, report it. Even if you’re not sure. Even if it’s “just” dizziness or a rash. The FDA doesn’t need you to be a doctor. They need you to be observant. A good report includes:
- The name of the drug, device, or product
- When you started using it
- When the problem started
- What happened - be specific
- What you did to fix it (e.g., stopped the drug, went to the ER)
- Your age and sex
- Any other medications or conditions you have
You can report online at www.fda.gov/medwatch, call 1-800-FDA-1088, or mail a form. The process takes 10 to 15 minutes. But it could help someone else avoid the same problem.
And if you’re a healthcare provider? Don’t wait for a perfect report. Submit what you have. A vague report is better than no report. The FDA can follow up. They can’t fix what they don’t know.
Is MedWatch only for drugs?
No. MedWatch covers all FDA-regulated products, including prescription and over-the-counter medicines, vaccines, medical devices (like pacemakers and insulin pumps), biologics, cosmetics, and even hemp-derived products. Any safety issue with these products can be reported.
Can I report a problem if I’m not a doctor?
Yes. Anyone can report - patients, family members, caregivers, or even bystanders. The FDA encourages public reporting because many serious side effects are first noticed by the people who use the products. You don’t need medical training to notice something unusual.
Do I need to prove the product caused the problem?
No. You don’t have to prove causation. The FDA’s job is to look for patterns. If multiple people report the same reaction, even if it seems unlikely, the agency investigates. It’s better to report something uncertain than to stay silent.
How long does it take for the FDA to act on a report?
There’s no fixed timeline. Some reports trigger immediate alerts - especially if they involve deaths or serious injuries. Others are part of larger trends that take months or years to confirm. For example, the Allergan breast implant recall happened in 45 days because of a clear signal. But for slower-developing issues, like long-term liver damage, it can take years of data.
Are reports anonymous?
Yes. You can file a report without giving your name. The FDA doesn’t require personal information, though providing contact details can help them follow up if they need more details. Your identity is protected under federal privacy rules.
What if I report and nothing happens?
Nothing happening doesn’t mean your report didn’t matter. The FDA receives over a million reports a year. A single report is rarely enough to trigger action. But when several people report the same issue, patterns emerge. Your report could be the one that tips the scale.
Final Thoughts
MedWatch isn’t glamorous. It doesn’t make headlines. But it’s one of the most important systems protecting public health in the U.S. It turns individual experiences into collective knowledge. Every report - whether from a doctor, a patient, or a pharmacist - adds to a larger picture. And that picture helps the FDA decide when to warn, when to restrict, or when to pull a product off the market. The system isn’t perfect. But it only works if people use it.