When your blood pressure stays too high for too long, it doesn’t just strain your heart and kidneys-it starts eating away at the tiny blood vessels in your eyes. This isn’t theoretical. It’s happening right now to millions of people who don’t even know their eyes are in danger. Hypertensive retinopathy is the silent thief of vision, creeping in without symptoms until it’s too late. And the worst part? You can’t feel it until your vision starts blurring, dark spots appear, or you wake up with half your sight gone.
What Exactly Is Hypertensive Retinopathy?
Hypertensive retinopathy is damage to the retina-the light-sensitive layer at the back of your eye-caused by long-term high blood pressure. The retina has a dense network of tiny blood vessels that supply oxygen and nutrients. When blood pressure stays elevated, these vessels get squeezed, thicken, leak, or even block off completely. Over time, this leads to bleeding, fluid buildup, and scarring in the retina. The result? Blurry vision, blind spots, or in severe cases, permanent blindness.
This isn’t a rare condition. About 13.9% of U.S. adults have stage 2 hypertension (140/90 mmHg or higher), according to CDC data from 2022. That’s roughly 34 million people. And of those, nearly 1 in 14 will develop some form of retinal damage from high blood pressure. The damage doesn’t happen overnight. It builds over years. But once it starts, it’s often irreversible.
The Four Stages of Retinal Damage
Doctors use the Keith-Wagener-Barker (KWB) system to grade the severity of hypertensive retinopathy. It’s not just a label-it’s a warning sign for your entire body.
- Grade 1: Mild narrowing of the retinal arteries. No bleeding or leakage yet. Many people have no symptoms. But if your blood pressure has been above 130/80 for more than 3 years, you could already be here.
- Grade 2: Arteries are noticeably narrower, and you’ll see arteriovenous nicking-where a thickened artery presses down on a vein like a thumb on a hose. This disrupts blood flow. At this stage, 22% of patients with uncontrolled hypertension show visible changes during a routine eye exam.
- Grade 3: Now you’re seeing hemorrhages (tiny bursts of blood), cotton wool spots (white patches from nerve damage), and hard exudates (yellowish lipid deposits). Vision may start to blur. This stage means your blood pressure has been out of control for at least 5 years.
- Grade 4: The most dangerous. Swelling of the optic nerve (papilledema) appears. This signals malignant hypertension-blood pressure above 180/120 mmHg. About 40% of people with this level develop optic nerve swelling within 72 hours. Up to 15% lose vision suddenly. These patients also have a 78% higher risk of stroke.
Grade 4 isn’t just an eye problem. It’s a full-blown medical emergency. Your heart, brain, and kidneys are already under extreme stress.
How Your Eyes Reveal What’s Happening Inside
Your retina is the only place in your body where doctors can see blood vessels without cutting you open. That’s why hypertensive retinopathy is called a “window to systemic vascular health.” The changes in your eye don’t just reflect high blood pressure-they predict what’s coming next.
Studies show that people with retinal damage from hypertension have a 2.5 times higher risk of heart attack or stroke. Arteriovenous nicking? That’s a 3.2 times higher risk of stroke. Cotton wool spots and hemorrhages? They’re tied to kidney disease and heart failure. The same vessels that are clogging in your eye are clogging in your brain and heart.
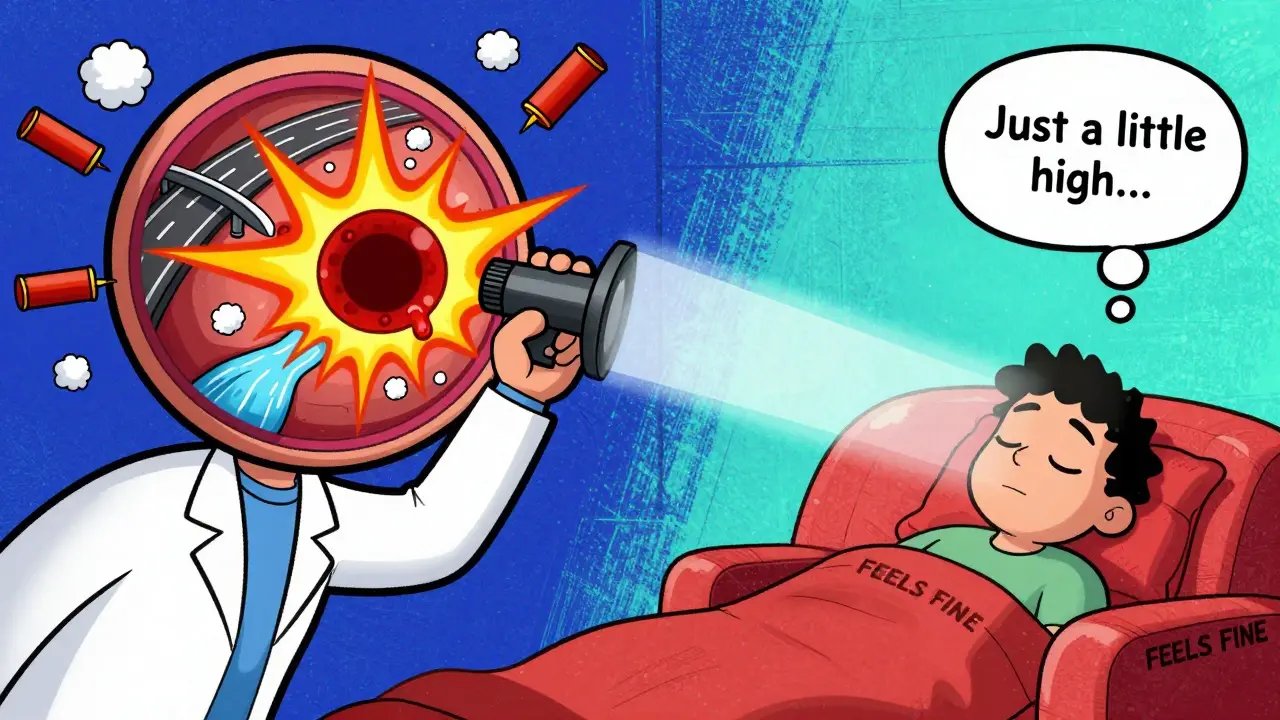
And here’s the scary part: You might not know you have it. About 68% of people with early-stage retinopathy (Grade 1-2) report no vision problems at all. They feel fine. Their blood pressure is “just a little high.” But the damage is already there. By the time they notice blurred vision or dark spots, it’s often Grade 3 or 4.
What Symptoms Should You Watch For?
Early on? Nothing. That’s the danger.
As it progresses, symptoms include:
- Blurred or dim vision
- Sudden loss of vision in one or both eyes
- Double vision
- Headaches, especially with high blood pressure spikes
- Seeing “curtain-like” shadows over your field of vision
- Dark spots or floaters that don’t go away
One Reddit user, u/RetinaWarrior, described waking up with dark spots in the center of his vision after his blood pressure hit 210/110. Another reported double vision and severe headaches during a hypertensive crisis. These aren’t rare stories. They’re clinical realities.
Most people wait 18 to 24 months before seeing a doctor about vision changes. Only 15% connect their blurry eyes to high blood pressure on their own. By then, the damage is often permanent.
How Doctors Diagnose It
There’s no blood test for hypertensive retinopathy. Diagnosis comes from a simple eye exam.
An ophthalmologist uses an ophthalmoscope to look directly at your retina. They’ll check for:
- Narrowing of arteries
- Arteriovenous nicking
- Flame-shaped hemorrhages
- Cotton wool spots
- Hard exudates
- Swelling of the optic disc
Advanced tools like optical coherence tomography (OCT) can measure retinal thickness. In exudative stages, thickness increases by 10-15%. AI systems like RetinaCheck AI, cleared by the FDA in 2022, now help detect these changes with 92% accuracy-up from 75% with the human eye alone.
Most major medical centers use the KWB grading system. But only 42% of community clinics do. That’s a gap. If your primary care doctor doesn’t check your retina during a hypertension visit, ask for a referral.

Can It Be Reversed?
Yes-but only if caught early.
Grade 1 and 2 changes can improve or even disappear with strict blood pressure control. Studies show that dropping systolic pressure by 25 mmHg within 48 hours resolves acute retinal damage in 65% of cases. Vision often starts improving within 7-10 days.
But Grade 3 and 4? The damage is often permanent. Hard exudates, nerve fiber layer loss, and optic nerve swelling can leave lasting blind spots. Even with perfect treatment, 22% of patients with advanced retinopathy never fully recover their vision.
Medications matter too. The European Society of Cardiology found that ACE inhibitors reduce retinal damage progression by 32% compared to calcium channel blockers. That’s a big difference. If you’re on blood pressure meds and your vision is worsening, talk to your doctor about switching.
What You Can Do Right Now
Don’t wait for symptoms. If you have high blood pressure, here’s your action plan:
- Get your eyes checked annually. Even if your vision is fine. The American Academy of Ophthalmology says Grade 1 changes can appear after just 3 years of uncontrolled hypertension.
- Check your blood pressure at home. Use a validated monitor. Track it daily. If your numbers are consistently above 130/80, you’re at risk.
- Know your numbers. Systolic pressure above 160 mmHg or diastolic above 120 mmHg means you’re in danger zone. Retinal hemorrhages appear in 35% of patients with systolic BP over 180 for 6+ months.
- Don’t ignore headaches or vision changes. If you wake up with blurred vision or dark spots, treat it like a heart attack. Call your doctor immediately.
- Ask about retinal screening. If you have resistant hypertension (BP still high after 3 medications), the American Heart Association now recommends exams every 6 months.
Patients who join programs like the American Heart Association’s “Check. Change. Control.” have 35% better blood pressure control. Why? Because they understand the link between their eyes and their heart.
The Future: Better Detection, Better Outcomes
Research is moving fast. The NIH launched the RETINA-HTN study in May 2023 to find genetic markers that predict who’s most vulnerable to retinal damage. Early results suggest 37 gene variants may identify high-risk patients before any damage occurs.
New devices like RetiFlow, which measures blood flow in retinal capillaries without dye or surgery, are entering clinical use. It’s 94% accurate compared to traditional methods. This could make screening as easy as a quick scan during a routine checkup.
And the market is responding. The global diagnostic market for hypertensive retinopathy is projected to hit $1.8 billion by 2027. More clinics will have AI tools. More doctors will screen. But until then, the responsibility falls on you.
High blood pressure doesn’t just kill quietly. It steals your vision quietly too. The eye doesn’t lie. If your retina is damaged, your body is in trouble. The good news? You can stop it-before it’s too late.
Can high blood pressure cause blindness?
Yes. Uncontrolled high blood pressure can lead to hypertensive retinopathy, which damages the retina’s blood vessels. In advanced stages (Grade 4), it can cause optic nerve swelling, bleeding, and permanent vision loss. About 22% of patients with severe retinopathy never fully recover their vision, even with treatment.
How long does it take for high blood pressure to damage the eyes?
Damage can begin after just 3-5 years of uncontrolled hypertension. Grade 1 changes-like mild artery narrowing-can appear in patients with blood pressure above 130/80 for over 3 years. By 5 years, many patients show signs of more advanced damage like hemorrhages or exudates.
Can you have hypertensive retinopathy without knowing it?
Absolutely. About 68% of people with early-stage retinopathy (Grade 1-2) have no symptoms. Vision stays normal until the damage is severe. That’s why routine eye exams are critical for anyone with high blood pressure-even if they feel fine.
Is hypertensive retinopathy reversible?
Early stages (Grade 1-2) can improve or reverse with strict blood pressure control. Vision may begin to improve within 7-10 days. But advanced stages (Grade 3-4) often cause permanent damage to the retina and optic nerve. Once scarring or nerve loss occurs, recovery is limited.
How often should someone with high blood pressure get an eye exam?
Annual eye exams are recommended for all patients with hypertension. If you have stage 2 hypertension (140/90 or higher), or if your blood pressure is resistant to treatment (still high after 3 medications), the American Heart Association now recommends exams every 6 months.
Can lifestyle changes reverse retinal damage?
Lifestyle changes-like losing weight, cutting salt, exercising, and quitting smoking-help lower blood pressure and slow or stop further damage. But they won’t undo existing scarring or nerve damage. Medication and close monitoring are still needed. The best outcome comes from combining lifestyle changes with prescribed treatment.
Wow. This is one of those posts that makes you stop scrolling and actually think. I had no idea your eyes could show you how bad your blood pressure is before you feel anything. I’m 42, been told I’m ‘pre-hypertensive’ for three years, and I’ve been ignoring it because I ‘feel fine.’ Now I’m scheduling an eye exam tomorrow. If your retina’s talking, you better listen. Thanks for laying it out like this-no fluff, just facts that could save your sight.
Ugh. Another ‘you’re gonna die if you don’t check your eyes’ scare post. I’m not gonna waste $200 on an eye exam because some guy on the internet said so. I eat salad once a week and I’m fine.
So if I’m reading this right-arteriovenous nicking = 3.2x stroke risk? That’s wild. I’ve been on lisinopril for 18 months but my BP still hovers around 145/92. I wonder if the exudates I saw in my OCT last year were from that. Anyone know if ACE inhibitors really outperform ARBs for retinal protection? The ESC paper mentioned 32% reduction, but I’ve seen conflicting data from the 2021 JAMA meta-analysis…
My uncle went blind in one eye from this. Didn’t know he had high BP until he woke up with a dark spot the size of a quarter. Now he’s on 5 meds and uses a cane. Don’t be him. Get checked. Seriously. It’s 10 minutes. You’re worth more than a ‘maybe later’.
This is so important. I’m so glad someone shared this. I used to think eye exams were just for glasses. Now I know they’re like a health dashboard. If you have high blood pressure, please, please, please get your eyes checked. It’s not scary-it’s empowering. You’re not weak for having high BP. You’re strong for doing something about it. You’ve got this.
Wait-so you’re telling me that if I ignore my BP for five years, my retina turns into a crime scene? And that AI tools now detect this better than human doctors? But only 42% of clinics even use the grading system? So… we’re relying on outdated practices while tech is 92% accurate? That’s not just negligence-it’s systemic failure. And you’re telling me to ‘ask for a referral’? What if I can’t afford it? What if I don’t have insurance? Where’s the policy change? Where’s the public health campaign? This isn’t a personal responsibility issue-it’s a structural one.
In India, we call this 'netri roga'-eye disease from pressure. Many people do not know that hypertension can affect eyes. My father had Grade 3 retinopathy before he was diagnosed. He was told to check BP only when he had headache. Now he sees better after treatment. Please tell your family. Eye check is not luxury. It is life.
I’m 38, BP’s been 138/88 for two years. No symptoms. But now I’m booking an eye appointment. Better safe than sorry. Thanks for the clear info.