Every year, over 1.5 million people in the U.S. are harmed by medication errors - and many of those mistakes happen because the label on your pill bottle doesn’t match what your doctor prescribed. It’s not always the pharmacy’s fault. Sometimes, the prescription gets typed wrong. Sometimes, two drugs look or sound alike. Sometimes, a decimal point gets lost. But here’s the truth: you are the last line of defense. No pharmacist, no barcode scanner, no automated system can catch every mistake - but you can.
What a pharmacy label should show
Before you even open the bottle, know what you’re looking for. A correct prescription label must include five key pieces of information:- The full drug name - both brand and generic (e.g., metoprolol succinate, brand name Lopressor)
- The strength - how much is in each pill or dose (e.g., 50 mg, 0.1 mg, 10 mL)
- The dosage form - tablet, capsule, liquid, patch, inhaler
- The directions - how often and how to take it (e.g., "Take one by mouth twice daily with food")
- The reason for use - what condition it’s for (e.g., "for high blood pressure")
Here’s the problem: only about 18% of community pharmacy labels include the reason for use. That’s a huge gap. If you don’t know why you’re taking a pill, you won’t know if it’s wrong. A 2016 study from the University of Arizona found that when the indication was printed on the label, patients caught wrong-medication errors 63% more often.
Watch out for look-alike, sound-alike drugs
Some drugs are almost impossible to tell apart by name alone. These are called LASA (Look-Alike, Sound-Alike) drugs. The FDA tracks over 1,500 risky pairs. A few common ones:- Cycloserine (for tuberculosis) vs. Cyclosporine (for organ transplants)
- Hydralazine (for high blood pressure) vs. Hydroxyzine (for anxiety or allergies)
- Glipizide (for diabetes) vs. Glyburide (also for diabetes)
- PremazinE vs. pROMethazine - notice the capital letters? That’s tall-man lettering.
Tall-man lettering uses capital letters to highlight the parts of drug names that differ. It’s meant to make errors obvious. But here’s the catch: only 45 out of 1,500 high-risk pairs have it on labels right now. Don’t wait for the pharmacy to fix it - check it yourself. If you see a drug name written all in lowercase, compare it to the name on your doctor’s prescription. If it looks too similar to another drug you’ve taken, pause. Ask.
Read the numbers out loud
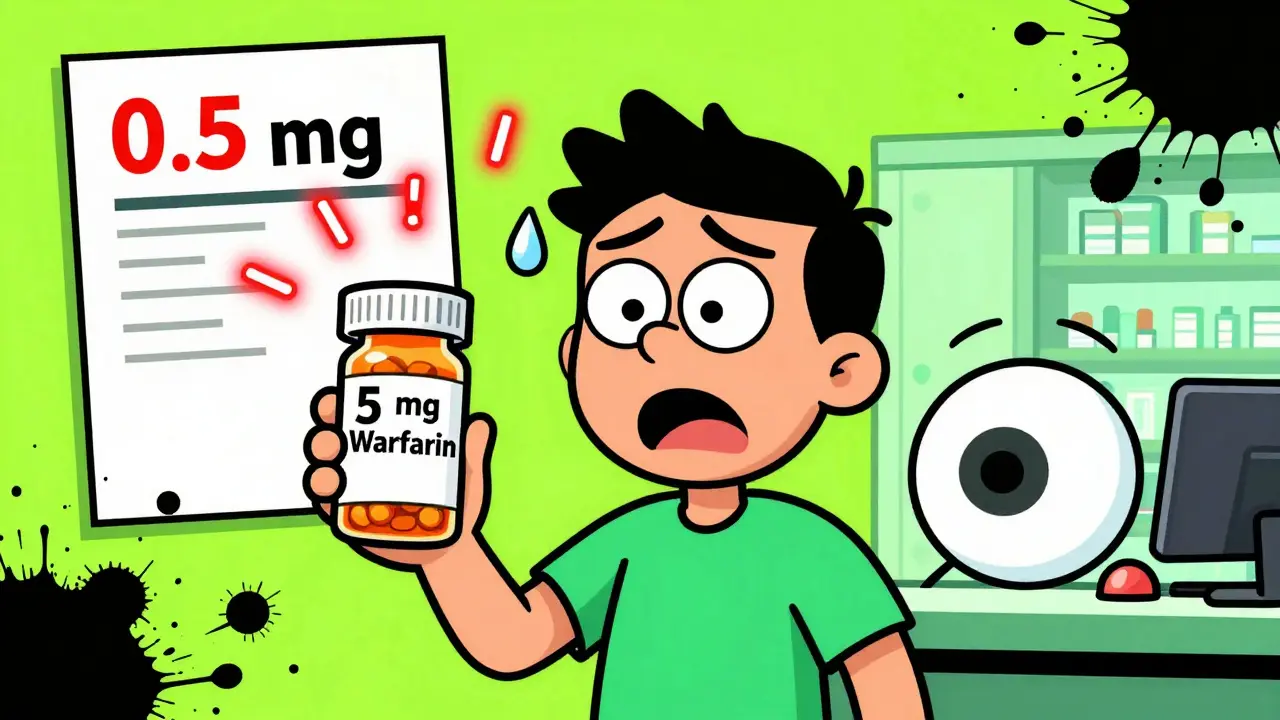
Strength errors are among the most dangerous. A misplaced decimal point can turn a safe dose into a deadly one. Warfarin, insulin, levothyroxine - these are high-alert drugs. One mistake can kill.Here’s what happened to a woman in Michigan: Her label said "5 mg" of warfarin. Her doctor prescribed 0.5 mg. She didn’t notice the missing zero. She took it. Within hours, she was bleeding internally. She survived - but barely.
Don’t just glance at the number. Say it out loud. "Five milligrams." "Zero point five milligrams." Your brain processes spoken words differently than written ones. A 2022 study from ISMP showed that reading the strength aloud caught 72% of decimal errors that were missed when reading silently.
If the label says "0.5 mg" and your doctor told you "half a milligram," that’s correct. If it says "5 mg" and you were told "half a milligram," that’s a 10x overdose. Stop. Don’t take it.
Compare it to your last bottle
If you’ve taken this medication before, your body remembers it. So does your brain - if you let it.When you get a refill, hold the new bottle next to the old one. Compare:
- Size and shape of the pill
- Color
- Imprint code (the letters or numbers stamped on the pill)
- Label wording
A 2021 study in the Journal of Patient Safety found that patients who compared their new prescription to their last bottle caught 89% of labeling errors. Those who didn’t compare? Only 42% caught anything.
Even if the label says "same as before," double-check. Pharmacies refill hundreds of prescriptions a day. Mistakes happen. A patient in Florida caught a mix-up between amoxicillin and azithromycin because the pills looked totally different - even though the label claimed they were the same.
Use the 4-step verification method
The Agency for Healthcare Research and Quality (AHRQ) created a simple, proven 4-step system. It takes 60 to 90 seconds. Use it every time.- Compare the label to your doctor’s prescription. Do they match exactly?
- Check for tall-man lettering. Are the key differences in the drug name capitalized? If not, ask if it’s the right one.
- Read the strength out loud. Say it. Hear it. Does it sound right?
- Confirm the directions. Does "take once daily" match what your doctor said? If the label says "take as needed" but your doctor said "take every day," something’s wrong.
Patients trained in this method caught 92% of simulated errors. Untrained patients? Only 55%. It’s not magic. It’s just attention.
Know your high-alert medications
Some drugs are more dangerous if messed up. The FDA lists these as high-alert medications. If you’re taking any of these, double down on verification:- Insulin
- Warfarin (blood thinner)
- Hydromorphone (opioid painkiller)
- Levothyroxine (thyroid hormone)
- IV potassium chloride
- Chemotherapy drugs
These six account for 65% of all serious labeling errors that lead to hospitalization or death. If you’re on one of these, treat every refill like it’s your first. Don’t assume. Don’t rush. Ask questions.
Technology can help - but don’t rely on it
New tools are popping up. CVS has a feature called "Label Lens" - scan the QR code on your prescription bag and hear an audio description of your meds. Apps like MedSafety Check use your phone’s camera to scan the label and compare it to the expected drug profile. One 2023 study found these apps catch errors with 94.7% accuracy.But here’s the problem: only 32% of community pharmacies use barcode scanning. Most still rely on humans typing in names and doses. And apps? They’re great - but they need you to start them. If you just grab the bottle and walk out, no app can save you.
Use tech as a backup. Not your main safety net.
Why people don’t check - and how to change that
A 2022 survey found that 58% of people don’t check their labels because they "trust the pharmacy." Another 32% say they "don’t know what to check."Here’s the truth: pharmacists are overworked. They’re filling 200+ prescriptions a day. Mistakes happen - even in the best-run pharmacies. Trust is not a safety protocol.
And you don’t need to be a doctor to check a label. You just need to know the five things listed above. You don’t need to be rude. You don’t need to argue. Just say:
"I just want to make sure this is right. Can you confirm the name and strength? My doctor prescribed [drug name] for [condition]."
That’s it. No confrontation. Just clarity.
A 2022 study in Annals of Internal Medicine found that 68% of patients who noticed something wrong still took the medication because they didn’t want to "bother" the pharmacist. Don’t be that person. Your life isn’t a bother.
What to do if you spot an error
If you see a mismatch:- Don’t take the medication.
- Call the pharmacy. Ask to speak to the pharmacist - not just the technician.
- Have your prescription number and doctor’s name ready.
- Ask: "Can you check the original prescription? I think there’s a mistake."
- If they dismiss you, call your doctor’s office. Ask them to confirm what they wrote.
Pharmacies are required by law to correct errors. You have every right to ask. If they refuse to fix it, file a report with your state board of pharmacy. Thirty-four states now require mandatory error reporting - your voice matters.
Final reminder
Medication errors don’t happen because you’re careless. They happen because the system is broken. But you’re not powerless. You’re the final checkpoint. The last person who can stop a mistake before it hurts you.Take 90 seconds. Ask two questions. Read the label out loud. Compare it to your last bottle. Trust your gut.
You’ve done the hard part - you’re taking your health seriously. Now protect it. One label at a time.

Oh wow, so now I’m supposed to become a pharmacy detective just to not die from a typo? Thanks for the 12-step survival guide for when capitalism outsources your safety to someone who’s been typing prescriptions since 7 AM with 37 other tabs open. I love how we’re told to ‘trust no one’ but also ‘don’t be rude.’ So what’s the polite way to scream at a pharmacist while they’re on their 200th script of the day? ‘Excuse me, could you please verify that this isn’t insulin instead of tylenol? I’m just trying to avoid becoming a human pincushion.’
i just read the label and take it. i trust the phamarcy. if they mess up its on them. i dont have time to be a pharmacist too. sorry but life is already hard enough.
Wow. A whole article on how to read a label. How quaint. I assume the author also believes in brushing your teeth and wearing seatbelts. Honestly, if you can’t distinguish between 0.5 mg and 5 mg, maybe you shouldn’t be managing your own meds at all. And don’t get me started on people who don’t know what ‘tall-man lettering’ is - it’s not a new age yoga pose. It’s a FDA safety feature. If you’re that lost, hire a caregiver. Or at least stop pretending you’re medically literate.
This is critical information, but it’s absurd that it even needs to be said. The fact that 82% of pharmacy labels omit the reason for use is a systemic failure, not a user error. In India, we often get handwritten prescriptions with no digital backup - and patients still catch errors because they ask. Why is the U.S. so far behind? Why is the burden placed on the patient instead of the system? This isn’t about vigilance - it’s about accountability. Pharmacies need mandatory digital verification, standardized labeling, and penalties for errors - not just a pamphlet telling people to ‘read out loud.’
I’ve been on warfarin for 7 years. I read the label out loud every time. I compare pills. I call if something looks off. And I’ve never once felt like a burden. The pharmacists I work with? They’re grateful. One even said, ‘You’re the reason we double-check.’ Don’t fear asking. Ask. It’s not rude - it’s responsible. And if someone makes you feel bad for it? They’re the problem, not you.
Oh sweetie, you really think your ‘4-step method’ is going to stop someone from taking 10x their dose? Honey, I’ve seen people take their kid’s ADHD meds because they didn’t check the label. You don’t need a checklist. You need a brain. And apparently, most people left theirs at home.
Great breakdown. I’ve been doing the compare-check-read-confirm thing since my mom had a mix-up with thyroid meds. It takes less than a minute. I do it with my parents too. They’re 72 and 75 - they don’t know all the drug names but they know what their pills look like. I showed them how to compare the old bottle. Now they do it together. Small habit. Big difference. You don’t have to be a genius. Just be consistent.
Let’s be real - if you’re on insulin or chemo and you don’t have a family member double-check your meds, you’re one typo away from a funeral. And don’t even get me started on how pharmacies print ‘take one daily’ on a bottle of 30 pills and then charge you $400 for it. The system is rigged. You’re not paranoid. You’re prepared. And if you’re still trusting a machine that’s been fed by a tired tech who just finished their 12th shift? You’re not just naive - you’re reckless.
I used to skip checking labels too. Until my dad almost took a double dose of metoprolol because the pharmacy swapped it with a similar-looking pill. He didn’t notice until his heart started racing. He’s fine now. But I still hold every new bottle up to the light and say the dose out loud. I don’t do it because I’m scared. I do it because I love him. And if you’re taking meds for your health - you owe it to yourself to be just as careful.