Imagine you’re rushed to the emergency room after falling at home. You’re in pain, confused, and can’t remember exactly what pills you took today. The doctor asks, "What medications are you on?" You say, "I think I take something for blood pressure... and maybe a vitamin?" That’s not enough. In fact, it’s dangerous. Half of all medication errors happen during transitions of care - like going from home to hospital, or from one doctor to another - because no one has a full, accurate list of what you’re taking.
Keeping a complete medication list isn’t just a good idea. It’s a safety necessity. And it’s something you can do yourself - right now - with no special tools or training. A real, up-to-date list saves lives. It stops bad reactions. It prevents doctors from prescribing something that clashes with what you’re already taking. And it cuts down on unnecessary tests, delays, and hospital visits.
What Goes on a Complete Medication List?
A simple note like "blood pressure pill" won’t cut it. You need details. Every single one. Here’s what a truly useful list includes:
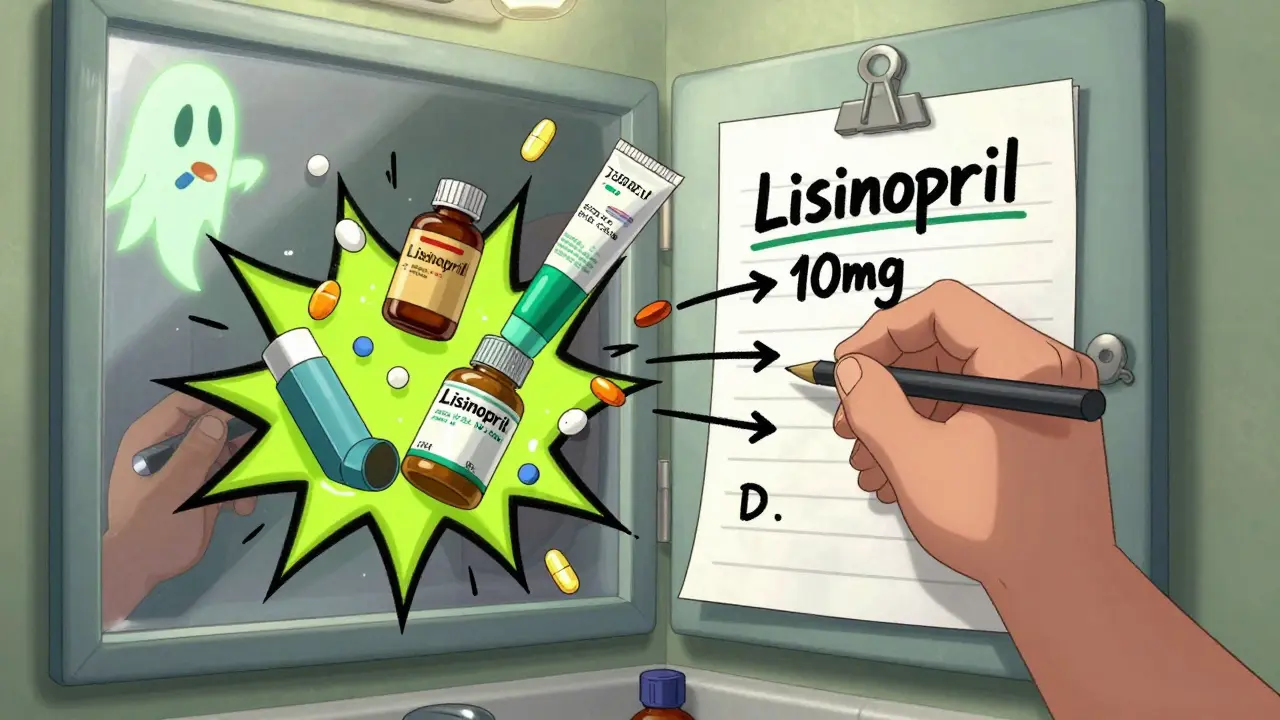
- Medication name - both generic and brand (e.g., lisinopril or Prinivil)
- Dosage - exactly how much you take (e.g., 10 mg, not one pill)
- How and when to take it - once daily with breakfast, as needed for pain, at bedtime
- Why you’re taking it - for high blood pressure, for arthritis pain, for sleep
- When you started - the date helps doctors spot patterns
- Who prescribed it - doctor’s name or clinic
- Refill status - when the next refill is due, or if it’s out
- Allergies and reactions - not just "penicillin allergy", but "amoxicillin - hives and swelling"
- Everything else - vitamins, supplements, herbal teas, eye drops, inhalers, creams, patches. Yes, even that turmeric capsule you take for your knees.
That’s it. No fluff. Just facts. And if you miss even one thing - say, your daily aspirin or that fish oil you got at the grocery store - you’re leaving a gap in your safety net.
Why Your Memory Isn’t Enough
Most people think they remember what they take. They don’t.
A study of 500 hospital admissions found that 73% of patient-reported medication lists had at least one major mistake - missing drugs, wrong doses, or wrong reasons. People forget OTC meds. They stop taking something but don’t tell anyone. They take a new pill for a cold and assume it’s not "real medicine."
And it’s not just seniors. A 2022 study in the Journal of General Internal Medicine found that 58% of patients - across all ages - forgot to mention over-the-counter drugs when asked. That’s more than half. If you’re one of them, you’re at risk.
Doctors aren’t mind readers. Nurses aren’t fortune tellers. They rely on what you tell them. If your list is incomplete, they’re guessing. And guessing with medications can kill.
How to Build Your List - Step by Step
Here’s how to make your list accurate and useful, in three simple steps:
- Collect everything. Go through every drawer, cabinet, and bag in your home. Pull out every pill bottle, box, tube, and packet. Write down each one using the full details above. Don’t skip anything. Not even the ginger tea you drink for nausea. Not even the eye drops you use once a week.
- Check with your pharmacy. Call your pharmacy - any pharmacy you’ve used - and ask them to print a full list of everything they’ve filled for you in the last year. Compare it to your list. Add what’s missing. Cross out what’s no longer taken.
- Review with your doctor. Don’t wait for your annual checkup. Schedule a 20-minute appointment just to go over your list. Bring a printed copy. Ask: "Is everything here still needed? Are any of these interacting?" Most doctors will be grateful you came prepared.
That first step - gathering everything - takes 20 to 30 minutes. It’s not fun. But it’s the most important 30 minutes you’ll spend on your health this year.
Paper or Digital? Which Works Better?
You don’t need an app. But you do need something reliable.
According to a 2022 survey by the National Council on Aging, 68% of patients still use paper lists. And that’s fine - if they’re kept current. A handwritten list on a notepad, kept in your wallet or purse, works perfectly well. Just make sure the writing is big enough to read. Use at least 12-point font if you print it.
Digital tools are growing fast. Apps like GoodRx, Medisafe, and MyTherapy let you scan barcodes, set reminders, and share your list with doctors through secure portals. As of mid-2024, 42% of GoodRx’s 150 million users actively use their medication list feature. These tools sync with your pharmacy and can alert you to interactions.
But here’s the catch: if you only use an app and your phone dies, or you forget it at home, you’re back to zero. That’s why experts recommend having both. Keep a printed copy with you. Use the app as a backup.
And if you’re not tech-savvy? Don’t stress. Paper is still the gold standard for safety. The FDA’s My Medicines guide, updated in January 2023, still recommends paper lists as the most accessible option - especially for older adults.
How This List Changes Your Care
A complete medication list isn’t just for emergencies. It transforms every interaction with the healthcare system.
When you walk into a new doctor’s office with your list, they don’t have to guess. They don’t have to call your old doctor. They don’t have to delay treatment waiting for records. They can start treating you - faster, safer.
Research from Harvard Medical School shows that patients who keep updated lists reduce their risk of serious adverse drug events by 43%. That’s not a small number. That’s life-changing.
For people with chronic conditions - diabetes, heart disease, arthritis - this list cuts down on hospital visits. The National Council on Aging found that patients who follow a simple routine of updating their list after every change reduce medication-related hospital admissions by 31%.
And it saves time. One practice in Ohio started requiring all patients to bring a current list to every visit. Within six months, their staff spent 2.7 fewer hours per provider per day chasing down medication histories. That’s time saved for real care - not paperwork.
Common Mistakes to Avoid
Even when people try, they mess it up. Here are the top errors - and how to fix them:
- Only listing prescriptions. Fix: Include everything - vitamins, supplements, creams, inhalers.
- Not updating after changes. Fix: Update the list the same day you start, stop, or change a medication. Keep a pen with your list.
- Using vague terms. Fix: Don’t write "pain pill". Write "ibuprofen 200 mg, one tablet every 6 hours as needed for pain".
- Forgetting "as needed" meds. Fix: Use a separate section labeled "PRN (as needed) Medications". Include how often you can take it and why (e.g., "lorazepam 0.5 mg, up to twice daily for anxiety attacks").
- Keeping it on your phone only. Fix: Always carry a printed copy. Don’t rely on cloud backups.
Also, don’t let anyone else update your list for you - not a caregiver, not a pharmacist, not a family member. You’re the only one who knows what you actually took today. They might assume. You know the truth.
What’s Changing in 2026
The system is slowly getting better. Thanks to the 21st Century Cures Act, all major health systems must now give you direct access to your full medication list through their patient portals. As of April 2024, 92% comply.
Medicare and Medicaid now penalize hospitals that don’t accurately reconcile patient medications. If your list is missing key items during admission, your hospital could lose up to 1.25% of its Medicare payments. That’s why more hospitals are pushing patients to bring their own lists.
And the future? Blockchain-based medication records are being tested. They’ll let you control who sees your list - and make sure it can’t be changed without your approval. But that’s years away. For now, your printed list is still the most powerful tool you have.
Start Today - No Excuses
You don’t need to wait for your next appointment. You don’t need to buy an app. You don’t need to be tech-savvy.
Right now, go to the medicine cabinet. Pull out every bottle. Write down the names, doses, and instructions. Add your allergies. Add your vitamins. Add your eye drops. Add your pain cream.
Print it. Put it in your wallet. Keep a copy at home. Show it to your doctor next time you see them. Update it every time something changes.
This isn’t busywork. It’s your shield. In a system full of gaps, your list is the one thing you control. And it could be the difference between walking out of the hospital - and not.
What if I take a lot of medications? Will my list be too long?
Length doesn’t matter - accuracy does. If you take 15 medications, your list will be long. That’s okay. In fact, it’s better. For patients with complex regimens, experts recommend color-coding: blue for heart meds, green for pain, red for allergies. You can also use icons - a pill for oral meds, a droplet for eye drops. A 2023 study found this improved adherence by 27%. The goal isn’t to make it pretty - it’s to make it impossible to miss anything.
Do I need to include supplements and herbal remedies?
Yes - absolutely. Supplements aren’t regulated like prescription drugs, so they can interact dangerously. St. John’s Wort can make your blood thinner ineffective. Grapefruit juice can cause toxic levels of cholesterol meds. Garlic pills can increase bleeding risk before surgery. If you take it, write it down. Even if your doctor says it’s "natural," it’s still medicine in your body.
How often should I update my list?
Update it immediately after any change - whether it’s a new prescription, a stopped pill, or a dosage change. Don’t wait for your next doctor visit. Set a monthly reminder on your phone: "Check meds". During that check, ask: Did I start anything new? Did I stop anything? Did my pharmacy refill something I didn’t take? Consistency beats perfection. Even a list updated once a month is better than one you update once a year.
What if I can’t read or write well?
You still need a list - just make it visual. Use pictures: draw a pill shape and write the name inside. Use stickers from pill bottles. Ask a family member, friend, or pharmacist to help you make a simple list with big letters and clear symbols. Many pharmacies offer free medication cards. Bring your bottles in and ask them to print one for you. The goal isn’t perfect handwriting - it’s clear communication.
Can I share my list electronically with my doctor?
Yes - and you should. Most major health systems now have patient portals where you can upload your list. If your doctor uses an electronic health record (EHR), they can import it directly. Ask your clinic if they accept digital lists. If they say no, print a copy and bring it. Many providers still prefer paper because it’s reliable. But if your system supports it, digital sharing saves time and reduces errors. The FDA and AMA both encourage using digital tools - as long as you have a backup.
What to Do Next
Don’t wait for the next emergency. Don’t wait for your next appointment. Right now, open your medicine cabinet. Pull out every bottle. Write down what’s inside. Use the checklist above. Print it. Put it in your wallet. Show it to your doctor.
If you’re helping someone else - a parent, a spouse, a friend - help them do the same. This isn’t about being perfect. It’s about being prepared. One complete list can prevent a hospital stay. One complete list can save a life.