When a pharmacist swaps a brand-name drug for a generic, it’s not just a cost-saving move-it’s a clinical decision. For most adults, it works fine. But for pediatric and senior patients, the stakes are higher. A pill that looks different, tastes bitter, or changes shape three times in a year can lead to missed doses, confusion, or even dangerous health outcomes. The truth is, generics are scientifically equivalent-but that doesn’t mean they’re the same in practice.
Why Generics Aren’t Always the Same for Kids
Pediatric medications aren’t just smaller versions of adult pills. Many brand-name drugs for children come as sweet-tasting liquids, chewable tablets, or sprinkle capsules designed for tiny mouths and developing systems. Generics? Often they don’t. According to the FDA, only 32% of generic pediatric formulations offer the same easy-to-take formats as their brand-name counterparts. That leaves 68% of kids stuck with pills or suspensions that taste awful or are hard to swallow. One parent on Reddit shared: "My 2-year-old threw up the generic amoxicillin because it tasted like chemicals. The brand-name version? He took it like candy." That’s not just a picky eater-it’s a treatment failure. When a child refuses medication, it’s not disobedience. It’s a formulation problem. And it gets worse. The FDA warns that many generic drugs used in children were never tested on kids at all. If a drug was approved for adults first, then went generic, there’s often no pediatric study behind it. That means dosing, absorption, and even side effects might not be fully understood for infants or toddlers. For example, switching from Prevacid (lansoprazole) to a generic omeprazole suspension for a 3-month-old with reflux is risky-omeprazole wasn’t even labeled for use under 1 year.What Seniors Face: Confusion, Change, and the Nocebo Effect
Seniors take an average of 4.8 prescription medications. That’s a lot of pills. When one of them changes color, shape, or size-especially multiple times in a year-it’s easy to panic. A 78-year-old in an AARP forum said: "I stopped taking my blood pressure pill because it looked different. I thought I got the wrong medicine." That’s not paranoia. It’s rational. The problem isn’t just appearance. It’s consistency. Seniors often rely on visual cues to remember what they’re taking. If their blood pressure pill goes from white oval to blue capsule to green tablet over six months, they may stop taking it altogether. A 2021 study found that 58% of seniors reported new side effects after switching to a generic-even when no pharmacological change occurred. This is the nocebo effect: expecting something to be worse makes you feel worse. And it’s not just about memory. Cognitive decline, vision problems, and hearing loss make explaining bioequivalence useless. Saying "it’s the same medicine" doesn’t help if the patient doesn’t understand what "bioequivalent" means-or if they can’t read the tiny print on the bottle.What Works: Clear, Simple, and Repeated Communication
The FDA and health experts agree: plain language is non-negotiable. Forget medical jargon. Use words like "same active ingredient," "same strength," and "same effect." Don’t say "therapeutic equivalence." Say: "This pill has the same medicine inside as your old one, just made by a different company. It’s cheaper, but just as safe." For kids, talk to the parent-not the child. Use the teach-back method: "Can you tell me how you’ll give this to your child?" Then listen. If they say, "I’ll crush it and mix it in applesauce," and the generic isn’t crushable, you’ve caught a problem before it starts. For seniors, involve caregivers. Use large-print handouts. Show them the old pill and the new pill side by side. Say: "This is your medicine. It changed shape, but the name on the bottle is the same. Here’s what changed-and what didn’t." Studies show that when pharmacists use the teach-back method with seniors, medication adherence improves by 32%. When parents are given visual aids and time to ask questions, 62% fewer refuse the generic.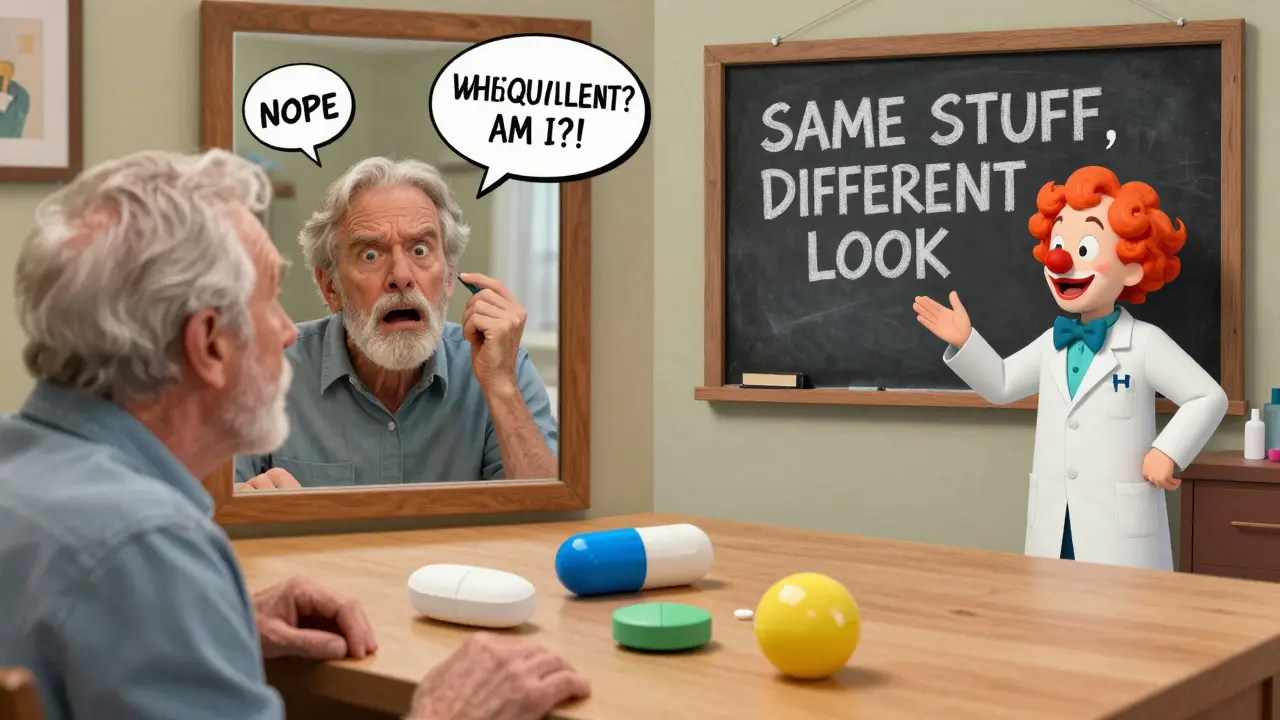
Don’t Assume Cost Is the Only Motivation
Many assume seniors take generics because they’re cheaper. That’s true-but not the whole story. A 2022 AARP survey found 45% of seniors accept generics because they trust the system. But 33% do it because they’re told they have to. That’s dangerous. When patients feel forced, they disengage. For parents, cost matters-but not as much as safety. A 2020 Pediatrics study found 62% of parents hesitate to switch to generics for their kids, not because they don’t want to save money, but because they fear their child’s condition won’t be controlled. That’s not irrational. It’s based on real experiences: taste aversion, vomiting, refusal, or relapse. The key is not to push generics. It’s to earn trust. Explain why the switch is happening. Say: "Your insurance requires a generic, but we’ve checked-it’s the same medicine. We’ll watch closely to make sure it works for your child."What You Must Avoid
Don’t say: "It’s the same thing." That’s not true. It’s the same active ingredient-but different fillers, coatings, and shapes. Those matter. Don’t assume the patient understands. Even if they nod, ask: "What part of this are you most worried about?" Don’t wait until the pharmacy counter to explain. If a substitution is coming, notify the provider first. Let them prepare the patient before the pill changes. Don’t ignore formulation differences. A liquid generic might use alcohol as a preservative. A chewable might have artificial coloring that triggers allergies. These aren’t minor details-they’re clinical risks.


Man, I never thought about how much kids hate the taste of generic antibiotics until now. My niece used to gag on the generic amoxicillin like it was poison. We switched back to the brand for a few months just so she’d actually take it. Worth the extra cash, honestly. Now she’s 8 and doesn’t care anymore, but back then? It was a nightmare.
I’ve seen this firsthand. My grandfather stopped taking his blood pressure med because the generic looked like a different color. He called the pharmacy three times. They told him it was ‘the same thing.’ He didn’t believe them. He didn’t trust them. He didn’t take it. And yes, he ended up in the ER. This isn’t a minor issue. It’s a systemic failure.
It’s wild how much formulation matters. I work in a clinic and we started keeping samples of both brand and generic on hand. Parents can see the difference-texture, color, even smell. It’s not about trust in science. It’s about trust in the person explaining it. When we show them side by side, they relax. They ask better questions. It’s small, but it works.
My mom’s 74 and takes eight pills a day. One month, her generic blood thinner changed from a white oval to a blue capsule. She stopped taking it for two weeks because she thought she got the wrong medicine. I had to sit with her for an hour, show her the bottle, the old pill, the new pill, the prescription label. She cried. Not because she was scared-because she felt ignored. No one asked if she understood. They just handed her the new bottle.
So we’re just supposed to baby these patients now? Adults can handle a pill change. Kids and seniors? We’re treating them like toddlers. Maybe if they weren’t so clingy to brand names, we wouldn’t have this problem. Insurance wants to save money. Why are we making it harder?
It is imperative to recognize that the therapeutic outcome is not solely contingent upon pharmacological equivalence. The psychological and cognitive dimensions of medication adherence are profoundly significant, particularly among vulnerable populations. The implementation of visual aids, caregiver involvement, and the teach-back methodology represents not merely a clinical best practice, but a moral imperative in patient-centered care.
in india we dont even have much generic options for kids. most are just adult pills crushed and given. no taste masking, no safe dosing. parents just hope it works. i wish more places had the same awareness as the us. this post is spot on.
Ugh. So now we’re gonna pamper every parent and grandparent who can’t read? If they can’t handle a pill changing shape, maybe they shouldn’t be managing meds. I’ve been on 12 different generics in 5 years. Never had an issue. Just take the damn pill.
Wait, so if a generic changes color every few months, and the senior stops taking it, is that really the nocebo effect? Or is it just common sense? I’d stop too. What if it’s a counterfeit? That’s not paranoia-that’s survival instinct. Maybe we need better tracking. Or at least a QR code on the bottle.