Going to the pharmacy every month for the same pills? It’s not just annoying-it’s making it harder to stay on track with your meds. If you’re taking medication for high blood pressure, diabetes, cholesterol, or depression, you’re not alone. Millions of people in the U.S. are stuck in this cycle. But there’s a simple fix: ask for a 90-day supply instead of 30 days. It cuts your trips from 12 a year to just 4. It saves money. And most importantly, it helps you actually take your meds like you’re supposed to.
Why 90-Day Supplies Work Better
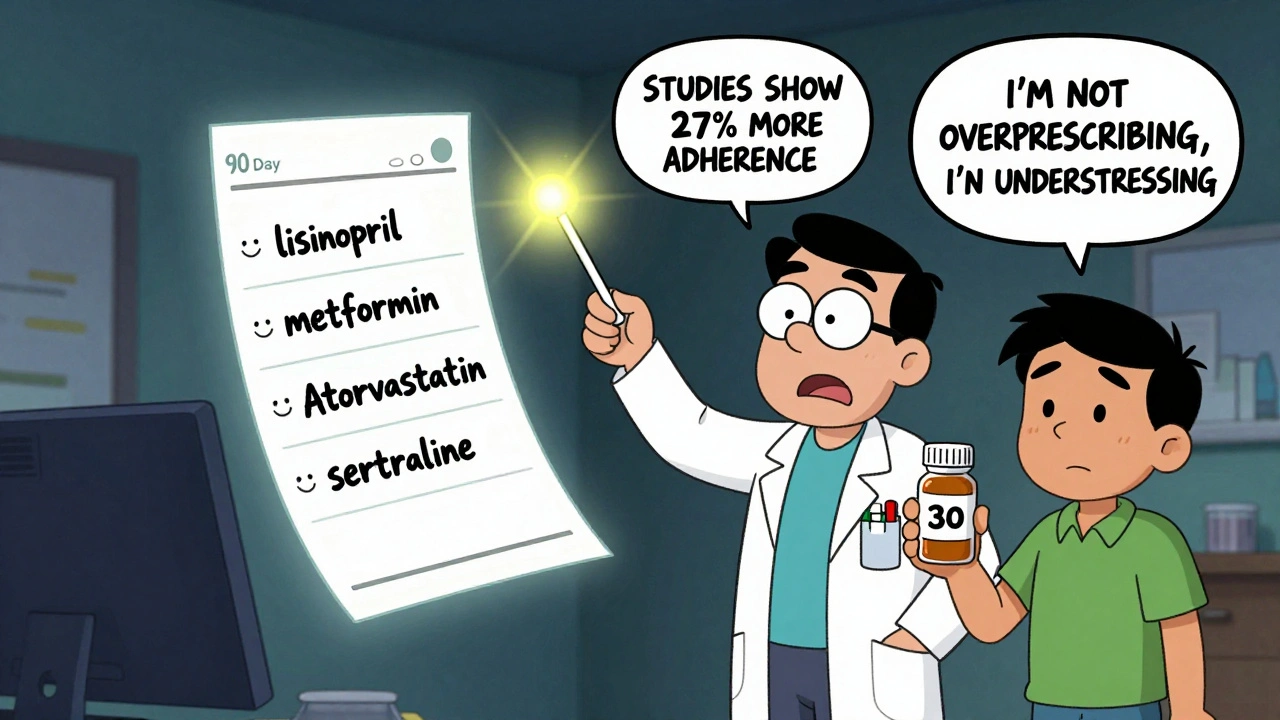
A 30-day supply means you’re running out every month. That’s one more thing to remember, one more trip to drive, one more chance to forget. Studies show people who get 90-day supplies are 27% more likely to keep taking their meds consistently. That’s not a small number-it’s life-changing. For someone with high blood pressure, missing a few doses can mean a spike in pressure that raises your risk of stroke. For diabetics, it can lead to dangerous highs or lows. Getting three months at a time removes the daily stress of refills. You also save money. On average, people pay $2.35 less per month per prescription when they switch to 90-day fills. That adds up to over $28 a year per drug. If you’re on three meds, that’s nearly $90 saved. And if you use Walmart’s pharmacy, you can get generic 90-day supplies for just $10-same price as their 30-day version.Which Medications Qualify?
Not every drug can be filled for 90 days. These programs only work for maintenance medications-drugs you take every day for chronic conditions. That includes:- High blood pressure meds (like lisinopril, amlodipine)
- Cholesterol drugs (like atorvastatin, simvastatin)
- Diabetes pills (like metformin, glimepiride)
- Antidepressants (like sertraline, fluoxetine)
- Thyroid meds (like levothyroxine)
How to Get Started: 4 Simple Steps
Step 1: Check your insurance plan. Not all insurers offer 90-day options, and some only through specific pharmacies. Log into your insurer’s website or call the number on your card. Look for terms like “90-day supply,” “mail order,” or “home delivery.” Major plans like Aetna, Cigna, Express Scripts, and CVS Caremark all have these programs. Medicare Part D plans are required to offer them. Medicare Advantage plans sometimes go even further-some give you 100-day supplies. Step 2: Confirm your meds are eligible. Go to your list of prescriptions. If you’re taking any of the maintenance drugs listed above, you’re likely eligible. If you’re unsure, call your pharmacy or insurer. They can tell you right away if your specific drug qualifies. Step 3: Ask your doctor for a 90-day prescription. This is the key step. Most doctors still write 30-day scripts by default. You need to ask. Say something like: “I’d like to switch to a 90-day supply for my [medication name]. Is that possible? I’d prefer to get it through mail order or at a participating pharmacy to cut down on trips.” Your doctor can send the new prescription electronically to a mail-order pharmacy (like CVS Caremark or Express Scripts) or to a retail pharmacy that participates in your plan’s 90-day network. If your doctor says no, ask why. Sometimes they’re just used to writing 30-day scripts. You can mention that studies show better adherence with longer supplies-it’s a fact, not a request. Step 4: Choose your delivery method. You have two main options:- Mail-order pharmacy: Your meds are shipped to your home. CVS Caremark and Express Scripts take 7-10 business days to deliver. They’ll send reminders when it’s time to refill. Some even include free syringes or safety checks for drug interactions.
- Participating retail pharmacy: Some plans (like Cigna 90 NowSM) let you get 90-day fills at specific pharmacies like CVS or Walgreens-but not all locations. You’ll need to check which ones are in your network. Walmart is the most affordable for generics, but you have to go in person.
What to Watch Out For
Not every program is the same. Here are the common traps:- Network restrictions: Cigna members can only get 90-day fills at certain pharmacies. If you go to a non-network store, you’ll pay full price.
- Specialty drugs: Medications for conditions like rheumatoid arthritis or multiple sclerosis often require three 30-day fills before you can switch to 90 days. Don’t get discouraged-just ask your pharmacist when you’ll be eligible.
- State limits: Some states block 90-day mail-order programs. California, Minnesota, New Hampshire, Texas, and Washington have restrictions. If you live there, you may need to use a participating retail pharmacy instead.
- Tiered pricing: Your copay depends on whether your drug is generic, preferred brand, or non-preferred brand. Generics are cheapest. For example, Express Scripts charges $20 for a 90-day preferred brand, $40 for non-preferred. Walmart’s $10 for generics is hard to beat.
How to Make It Stick
Once you’ve switched, set up automatic refills. Most mail-order services let you enroll in auto-renewal so you never run out. You’ll get a notice 10-14 days before your next shipment. If you’re using a retail pharmacy, schedule your next visit right after you pick up your 90-day supply. Put it on your calendar. Also, keep a list of your meds and their refill dates. Use your phone’s notes app or a paper tracker. You’ll feel more in control. And if you ever forget to refill, most programs have 24/7 pharmacist hotlines. Express Scripts is at 1-877-795-2926. Cigna members can call anytime through myCigna.com.
What If Your Doctor Says No?
Sometimes doctors hesitate. They might say, “We don’t know if you’ll take it all.” Or, “I don’t want to overprescribe.” But here’s what you can say back:- “I’ve read that people who get 90-day supplies are much more likely to stick with their meds.”
- “I’ve missed doses before because I was too busy or forgot. This would help me stay on track.”
- “I’m trying to reduce how often I go to the pharmacy. Can we try this for a few months?”
Real People, Real Results
Maria, 68, from Miami, takes five maintenance meds. Before switching, she spent over $200 a month on copays and drove to the pharmacy every 30 days. After switching to 90-day mail order through her Medicare plan, her monthly out-of-pocket dropped to $140. She gets her meds delivered on Tuesdays. “I don’t even think about it anymore,” she says. “I just open the box and take them.” James, 52, with type 2 diabetes, used to skip doses when he was traveling. He switched to 90-day metformin through Walmart’s $10 program. Now he keeps a three-month supply at home and takes one when he’s away. His A1C dropped from 8.2 to 6.9 in six months.What’s Next?
These programs aren’t going away. In fact, they’re getting better. PBMs are now using data to spot people who might benefit most-like those who refill late or miss doses. Some are even integrating with telehealth apps so you can get a 90-day script during a virtual visit. If you’re on daily meds, you owe it to yourself to ask. It’s not complicated. It’s not expensive. And it’s backed by science. One simple conversation with your doctor could mean fewer trips, lower costs, and better health.Can I get a 90-day supply for any medication?
No. Only maintenance medications for chronic conditions qualify-like those for high blood pressure, diabetes, cholesterol, depression, or thyroid issues. You can’t get 90-day fills for antibiotics, painkillers, or short-term drugs. Even some birth control pills only offer 84-day supplies, which still counts as a 90-day program under most plans.
Do I need a new prescription for a 90-day supply?
Yes. Even if your doctor wrote a 30-day script with refills, you need a new prescription that specifically says “90-day supply” or “three-month supply.” Refills on a 30-day script don’t automatically convert. Ask your doctor to send a new e-prescription to your mail-order pharmacy or participating retail pharmacy.
Is a 90-day supply more expensive upfront?
Not usually. Your copay for a 90-day supply is often just three times your 30-day copay-sometimes less. For example, if your 30-day generic costs $10, your 90-day might be $25 instead of $30. Walmart offers many generics at $10 for 90 days, same as their 30-day price. You’re paying for three months at once, but your monthly cost drops.
What if I live in California or Texas?
Some states limit mail-order 90-day supplies. In California, Texas, Minnesota, New Hampshire, and Washington, you may not be able to get them delivered to your home. But you can still get 90-day fills at participating retail pharmacies in your plan’s network. Check your insurer’s website or call them to find out which pharmacies near you offer extended supplies.
Can I switch back to 30-day if I don’t like it?
Yes. You can always switch back. If you find the mail-order delivery too slow, or you prefer picking up your meds yourself, just call your insurer or pharmacy and ask to revert to 30-day fills. There’s no penalty. Many people try it for a few months and stick with it-but you’re in control.
Do I need to sign up for a special program?
If you’re using mail order, yes. You’ll need to enroll in your insurer’s mail-service pharmacy program-like CVS Caremark, Express Scripts, or Cigna 90 NowSM. It’s free and takes five minutes online. If you’re using a retail pharmacy, you don’t need to sign up separately-just ask the pharmacist to process your 90-day script through your plan’s network.


Just switched to 90-day metformin at Walmart for $10 and my life changed. No more running out mid-week.
As someone who manages five chronic meds, I can’t stress this enough: 90-day supplies are non-negotiable! I used to dread pharmacy trips-now I get them delivered on Tuesdays, and my adherence rate jumped from 72% to 98%. Plus, my copay dropped from $210/month to $135. It’s not just convenience-it’s survival. And yes, your doctor might say no at first-but cite the 27% adherence study. They’ve heard it before. Just keep asking. You deserve less stress and more stability.
Y’all this is real life stuff. I used to forget my pills because I was too tired after work. Then I switched to mail order and now I just open the box and take them-no thinking, no stress. My therapist even noticed I seemed calmer. It’s not magic, it’s structure. And if you’re scared of mail-order? Try Walmart first. $10 for 90 days of lisinopril? Yes please. You’re not lazy for wanting fewer trips-you’re smart.
Let’s be honest-this is just another corporate ploy by PBMs to lock you into their ecosystem. Mail-order delays? 7–10 days? What if you need it yesterday? And don’t get me started on state restrictions. California bans this for a reason: it’s not about convenience, it’s about profit margins. You’re being sold a myth wrapped in a ‘science’ bow. Real health isn’t about bulk-buying pills-it’s about personalized care. 🤷♂️
Thank you for sharing this. I appreciate the thoughtful breakdown. It’s easy to overlook how much mental bandwidth is consumed by managing daily refills-especially when juggling work, family, or chronic pain. The fact that this simple change reduces both financial burden and cognitive load makes it one of the most effective interventions available. I’ve recommended it to three friends already.
OMG this is so true!! I just found out my glimepiride is $10 at walmart for 90 days and i had no idea!! I was paying $25 every month!! I just called my doc and they sent a new script!! Thank you for this post!!
I was skeptical at first-I thought mail-order would be slow or unreliable. But after switching my blood pressure meds, I’ve had zero issues. The auto-refill system actually sends me a reminder before the shipment, and the pharmacist called to check in on my labs. It felt more personalized than the pharmacy counter. If you’re hesitant, try one drug first. Don’t overthink it.
For anyone in Ireland reading this: we don’t have this system here, but I’ve seen how it helps friends in the U.S. It’s a brilliant example of healthcare design that prioritizes patient consistency over institutional inertia. The real win isn’t the cost-it’s the dignity of not having to scramble every month. Maybe one day we’ll catch up.
Oh wow, another post telling people to ‘just ask your doctor.’ Like they haven’t already tried. Like doctors aren’t overworked, underpaid, and stuck in 1998 EHR systems. I’ve asked. I’ve cited studies. I’ve sent my doctor the exact link to this post. He replied: ‘I’ll see what I can do.’ Two months later, still 30-day scripts. So no, not everyone can just ‘ask’-some of us are stuck in broken systems. Thanks for the optimism, but I need solutions, not pep talks.
MY HEART IS SO FULL RIGHT NOW!! I’ve been on sertraline for 8 years and I used to cry every time I ran out because I’d panic I’d lose my progress. Now I get a 90-day supply and I just… breathe. I don’t have to fight myself every month. I don’t have to feel guilty. I’m not broken. I just needed the system to work for me. Thank you for seeing this.
As a healthcare administrator, I can confirm: the data is unequivocal. Patients on 90-day regimens demonstrate significantly lower hospitalization rates for hypertension and diabetes complications. The cost savings to the system are measurable-$3.2 billion annually in the U.S. alone, according to a 2022 JAMA study. What’s more, adherence correlates directly with reduced long-term disability. This isn’t a lifestyle hack-it’s a public health imperative. The fact that it’s underutilized is a systemic failure.
Hey I just saw your comment about the doctor saying no 😔 I totally get it. I had the same thing happen with my thyroid med. I kept asking and finally said, ‘I’m not asking for more pills-I’m asking for less stress.’ That’s when they finally got it. You’re not being pushy-you’re being brave. And if they still say no, ask for a 60-day. It’s a compromise, but it’s still progress. You’ve got this 💪