When you’re on home oxygen therapy, your life doesn’t stop-it just changes. You still cook, walk the dog, watch TV, and hug your grandkids. But now, every action comes with new rules. One wrong move, one spark near your oxygen equipment, and the consequences can be deadly. Oxygen isn’t flammable, but it makes everything else burn faster. And it doesn’t take much: a cigarette, a spark from a blanket, a hair dryer too close to the tubing. These aren’t hypothetical risks. In the U.S. alone, fire departments respond to nearly 2,500 home fires each year involving oxygen equipment. People die. Homes burn. It doesn’t have to be that way.
Know Your Oxygen System
There are three main types of home oxygen systems, and each has its own risks and handling rules. Most people use an oxygen concentrator. It plugs into a wall outlet, pulls oxygen from the air, and delivers it through tubing. These are quiet, low-maintenance, and don’t run out like tanks-but they need electricity. If the power goes out, you need a backup. Medicare requires all covered concentrators to have at least a 30-minute battery backup. If yours doesn’t, ask your provider for one. Compressed gas cylinders are metal tanks filled with oxygen under pressure. They’re portable but dangerous if dropped or exposed to heat. A damaged valve can turn the tank into a rocket-propelling it at 150 miles per hour. These tanks come in sizes from small M2 (1.5 lbs) to large G cylinders (170 lbs). Never store them in a hot car, near a radiator, or in direct sunlight. Temperatures above 125°F can cause pressure buildup and rupture. Liquid oxygen systems store oxygen as a super-cold liquid at -297°F. They’re lightweight and hold a lot of oxygen-up to 60 hours at 2 liters per minute-but they’re tricky. Spills can cause severe cold burns. The vapor can also pool near the floor and ignite if it reaches an ignition source. These systems are great for active users but require careful handling and regular refills.Fire Safety: The 10-Foot Rule
The old advice said to stay 5 feet away from open flames. That’s not enough. New research from the American Thoracic Society shows fires spread 3.7 times faster in oxygen-rich air. Smoke from a cigarette can ignite within half a second near tubing. The current standard? Stay 10 feet away from any open flame or heat source. That includes candles, fireplaces, stoves, grills, and even campfires on the porch. Don’t smoke. Not even outside. Not even if you think you’re far enough. If you must smoke, get off oxygen for at least 15 minutes and wait until the air clears. But the safest choice? Quit. Smoking and oxygen therapy don’t mix. Studies show 92% of oxygen-related deaths involve smoking within 5 feet of equipment. Electrical devices are just as dangerous. Hair dryers, electric razors, and space heaters can create sparks-even if they look fine. The FDA found that 41% of oxygen fires involve appliances within 3 feet of the equipment. Keep them out of the room when you’re on oxygen. Use battery-powered razors. Plug your concentrator into a dedicated outlet-no power strips, no extension cords. Overloaded circuits can overheat and spark.Bedding, Clothing, and Static Electricity
You might not think about your sheets or sweater, but they can start a fire. Synthetic fabrics like polyester, nylon, and acrylic build up static electricity. At just 1,000 volts, that static can spark-and you won’t even feel it. Humans don’t feel static until it hits 3,500 volts. That means you could be walking across your carpet, getting ready for bed, and unknowingly creating a spark right next to your oxygen tubing. Solution? Wear 100% cotton clothing and use 100% cotton bedding. Avoid wool blankets, fleece pajamas, and synthetic sheets. The American Lung Association recommends flame-resistant cotton blankets as part of an Oxygen Safety Kit. These kits also include warning signs, 10-foot zone markers, and fire extinguisher instructions. Ask your provider for one. If they don’t offer it, call the American Lung Association directly-they’ll mail you a free kit.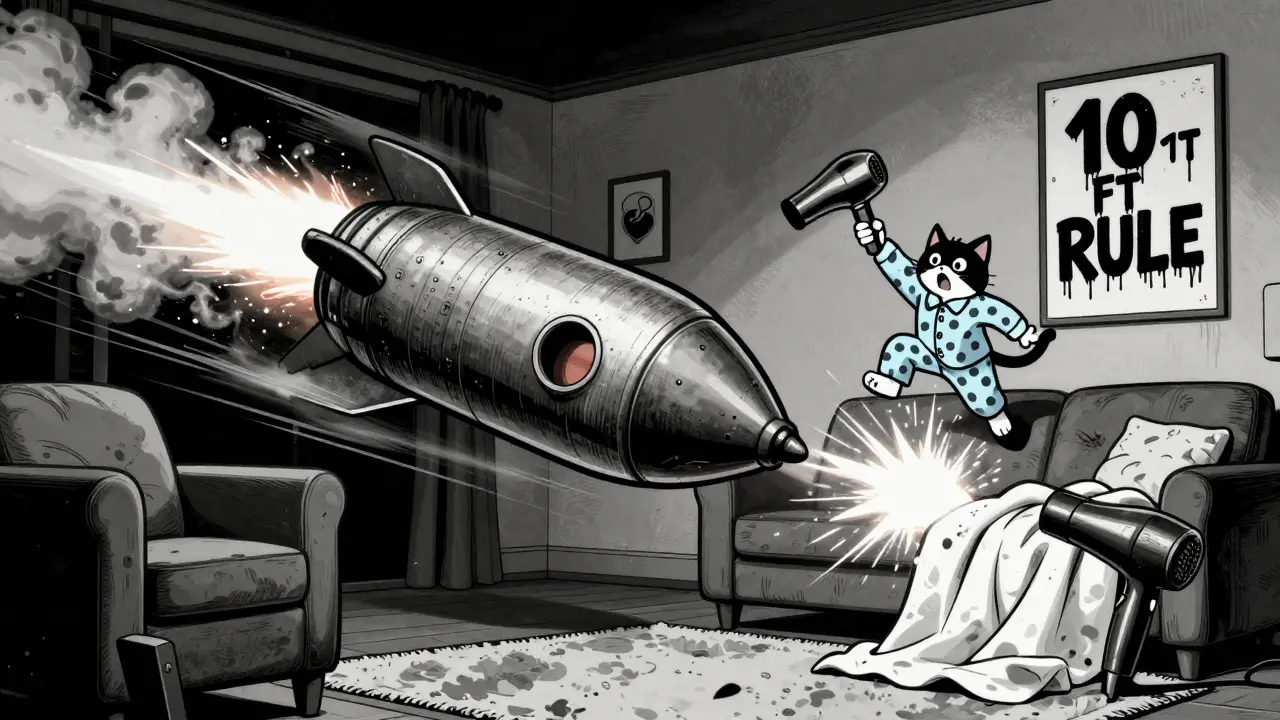
Managing Tubing and Mobility
Tripping over oxygen tubing is one of the most common accidents. A 2023 survey found 76% of users have tripped or nearly fallen because of their tubing. That’s not just a nuisance-it’s dangerous. Falls can knock over oxygen tanks, disconnect tubing, or cause injury. Fix it with simple tricks. Use ceiling-mounted tubing systems if your home allows it. If not, run the tubing along baseboards and secure it with Velcro straps or adhesive clips. Don’t tape it to the floor-that’s a tripping hazard. Many users attach their concentrator to a wheeled cart so it moves with them. That way, you’re not dragging 10 feet of tubing behind you. For active users, portable oxygen concentrators (POCs) are a game-changer. They’re small, lightweight, and approved for air travel. Brands like Inogen and Philips offer models that run on batteries for 4-8 hours. Always carry extra batteries when you leave home. Never let your POC sit in a hot car. Heat kills batteries and can damage the internal sensors.What to Do in an Emergency
If you see smoke or flames near your oxygen equipment, act fast. Don’t try to put it out yourself unless it’s tiny. Your priority is to get away and call 911. Step 1: Turn off the oxygen flow at the source. On a concentrator, press the power button. On a tank, close the valve. Don’t yank the tubing-that can cause more sparks. Step 2: Get out. Leave the house. Don’t stop to grab anything. Oxygen fires spread faster than you think. Step 3: Call 911 from outside. Tell them you’re on oxygen therapy and there’s a fire. That changes how they respond. Keep a fire extinguisher rated for electrical and flammable gas fires (Class ABC) near your oxygen setup. Know how to use it. If you’re unsure, ask your provider to show you during your next visit.Activity Guidance: Living Fully on Oxygen
Oxygen therapy isn’t a sentence-it’s a tool. You can still do most of the things you love. Walk. Travel. Gardening. Even swimming, if your system allows it. But you need to plan ahead. For short trips: Use a portable oxygen concentrator with extra batteries. Pack your tubing, spare nasal cannulas, and a backup tank. Always have a list of your oxygen settings (e.g., 2 LPM continuous) and your doctor’s contact info. For air travel: Call your airline at least 48 hours in advance. Not all POCs are allowed. Only FAA-approved models are permitted on planes. Check the FAA’s list of approved devices before you book. For outdoor activities: Avoid windy days if you’re using liquid oxygen-it evaporates faster. In cold weather, keep your concentrator warm. Moisture can freeze in the tubing. Use a humidity bottle if your provider recommends it. For sleep: Don’t change your oxygen flow without your doctor’s order. Many people need higher flow at night. If you wake up gasping, your settings might be too low. Don’t guess-call your provider.Who Should You Trust?
Not all oxygen suppliers are the same. A 2022 survey by the COPD Foundation found that 67% of patients received little or no safety training. Some providers just drop off equipment and leave. Others offer full training, follow-up calls, and safety checklists. Look for providers with high ratings on Trustpilot or Google. Apria Healthcare, for example, has a 4.3 out of 5 rating with over 1,800 reviews. Ask: Do they give you a written safety guide? Do they test your understanding before leaving? Do they offer annual safety refresher sessions? Medicare-certified suppliers are required to give you CMS Form 483 with 12 specific safety instructions. If they don’t, ask for it. If they refuse, report them to Medicare.What’s Changing in 2025
The rules are getting stricter-and safer. Starting in 2025, all new oxygen equipment sold in the U.S. must shut off automatically within half a second if it detects a flame. New smart concentrators, like the Philips Respironics SimplyGo Mini+, use AI to detect flames up to 18 inches away with 99.2% accuracy. These devices are already available and covered by Medicare in many cases. CMS is also launching its Oxygen Safety Verification Program in 2024. Every Medicare beneficiary on oxygen will need to pass an annual safety competency test. It’s a 20-minute online module. If you fail, your oxygen supply can be paused until you complete it. This isn’t a punishment-it’s a lifesaver.Final Thoughts: You’re Not Alone
Over 1.5 million Americans use home oxygen therapy. You’re not the only one navigating this. Millions have learned how to live safely with oxygen. The key isn’t fear-it’s knowledge. Learn the rules. Ask questions. Use the safety kits. Stick to cotton. Keep 10 feet clear. Test your fire extinguisher. Change your filters every 2-4 weeks. Service your concentrator every 6 months. This isn’t about restriction. It’s about freedom. With the right safety habits, you can still take walks in the park, visit family, and enjoy quiet evenings at home. Oxygen isn’t your enemy. Ignorance is. Stay informed. Stay safe. Keep living.Can I use an electric blanket while on home oxygen therapy?
No. Electric blankets generate heat and can create sparks from wiring or overheating. Even if they’re turned off, residual heat or electrical faults can ignite oxygen-rich air. Use a cotton comforter or heated mattress pad designed for medical use instead. Always keep electric blankets at least 10 feet away from oxygen equipment.
Is it safe to use a humidifier with my oxygen concentrator?
Yes, but only if it’s designed for oxygen use. Standard humidifiers can introduce bacteria or contaminants into your oxygen stream. Use only sterile water and a humidifier bottle approved by your provider. Clean it daily with vinegar and water, and replace the bottle every 3 months. Never use tap water-it can cause mineral buildup and damage the system.
How often should I clean my oxygen concentrator filter?
Clean the air filter every 2-4 weeks, depending on dust levels in your home. Remove it, rinse under lukewarm water, shake off excess, and let it air-dry completely before reinserting. Never use soap or a dryer. A dirty filter reduces oxygen purity and forces the machine to work harder, shortening its lifespan. Replace the filter every 6-12 months.
Can I travel with my oxygen concentrator on a plane?
Yes, but only if it’s FAA-approved. Check the FAA’s list of permitted devices before booking. You must notify the airline at least 48 hours in advance and bring enough batteries to last 150% of your flight time. Never check your concentrator as luggage-it must be with you in the cabin. Bring your prescription and a letter from your doctor in case you’re questioned.
What should I do if my oxygen concentrator stops working?
First, check the power cord and outlet. Plug something else in to confirm the outlet works. If it’s battery-powered, replace the battery. If the machine still doesn’t work, switch to your backup oxygen tank immediately. Then call your supplier. Don’t wait until you’re struggling to breathe. Most providers offer 24/7 emergency support for equipment failures. Keep their number taped to the concentrator.
Are there any foods or drinks I should avoid while on oxygen therapy?
No specific foods or drinks interfere with oxygen therapy. However, avoid alcohol and sedatives-they slow your breathing and can reduce oxygen levels in your blood. Also, avoid using aerosol sprays like hairspray or perfume near your oxygen equipment. A single spray can ignite instantly in an oxygen-rich environment. Use non-aerosol alternatives like roll-ons or pump sprays.
Can I use essential oils or aromatherapy with oxygen therapy?
No. Essential oils are highly flammable. Diffusers, candles, and oil warmers create heat and vapor that can ignite in oxygen-rich air. Even if you think you’re far away, the scent particles can mix with oxygen near your tubing. Stick to non-flammable alternatives like unscented lotions or natural ventilation.


Just got my new Philips SimplyGo Mini+ last week. The flame detection feature is insane-it shuts off within milliseconds if it senses anything even close to a spark. No more sweating over candles at Thanksgiving. Medicare covered it after I submitted the form. If you’re on oxygen and your device doesn’t have this, demand an upgrade. It’s not a luxury-it’s a lifeline.
10-foot rule is non-negotiable. I used to sit on the couch with my tank and smoke outside-thought I was fine. One day, my blanket sparked from static and the tubing caught fire. Didn’t burn down the house, but I lost my favorite chair. Now I wear cotton 24/7. No exceptions.
OMG I just found out my humidifier bottle was full of tap water 😱 I’ve been doing this for 3 years. Thank you for the warning! Just ordered a new one with sterile water. Also bought cotton sheets and threw out my fleece pajamas. 🙏
So let me get this straight-using essential oils is a death sentence, but I can still use a space heater if it’s 11 feet away? That’s like saying you can’t drink poison but you can sip it from a distance. Real helpful advice, guys.
I’m from South Africa and we don’t have the same oxygen infrastructure here, but I’ve seen what happens when people don’t respect the rules. My cousin lost his home in a fire caused by a hair dryer and an oxygen tank. He survived, but his wife didn’t. The 10-foot rule isn’t bureaucracy-it’s the difference between a Tuesday and a funeral. Please don’t gamble with this.
There’s a deeper truth here: oxygen therapy doesn’t just change how we live-it forces us to confront our relationship with control. We used to take breath for granted. Now, every movement is calculated. Every fabric, every outlet, every spark is a question of survival. But in this hyper-awareness, we rediscover presence. The cotton sheets aren’t just fireproof-they’re a ritual of mindfulness. The silence of the concentrator? That’s the sound of life, quietly humming. We aren’t being restricted. We’re being invited into a more deliberate way of being. And that’s a gift, even if it comes wrapped in fear.
Let’s be real-the real danger isn’t the oxygen. It’s the people who think they’re too cool for safety. You’re not special. You’re not ‘careful enough.’ You’re not ‘just this once.’ 92% of deaths involve smoking near oxygen. That’s not an accident. That’s negligence dressed up as rebellion. And if your provider didn’t give you CMS Form 483, they’re breaking federal law. File a complaint. Don’t wait for a funeral to wake up.
Y’all act like oxygen is some kind of magic potion from NASA. Nah. It’s just gas. But you know what’s worse? The corporate BS. They sell you $2000 concentrators then charge you $50 for a stupid cotton blanket. And don’t get me started on the ‘Oxygen Safety Verification Program’-sounds like a government tax on being sick. I’ve been on this for 7 years. I know what I’m doing. I don’t need a 20-minute quiz to prove I’m not an idiot. They’re treating us like toddlers with a death wish.
My grandpa’s on oxygen and he still smokes outside… but he waits 20 mins after he’s done. He says he’s fine. I told him he’s lucky he hasn’t blown up yet. He laughed. I didn’t. Just wanted to say-don’t be like my grandpa. Please. I love him too much to lose him.