Most people don’t talk about hemorrhoids-until they have them. Then it’s all you can think about. The itching, the pain, the embarrassment. You might try to ignore it, hoping it goes away. But if you’ve noticed bright red blood on your toilet paper or a tender lump near your anus, you’re not imagining it. Hemorrhoids are common-about 75% of people will deal with them at some point in their lives. The good news? They’re treatable. The better news? You don’t have to suffer in silence.
What Exactly Are Hemorrhoids?
Hemorrhoids aren’t some strange, rare condition. They’re normal blood vessels in your rectum and anus that help with stool control. Think of them like little cushions. But when they get swollen from pressure-maybe from straining during a bowel movement, sitting too long, or even pregnancy-they become a problem. That’s when you feel the discomfort. There are two main types: internal and external. They’re not just different in location-they’re different in how they behave, what they feel like, and how they’re treated.Internal Hemorrhoids: The Silent Ones
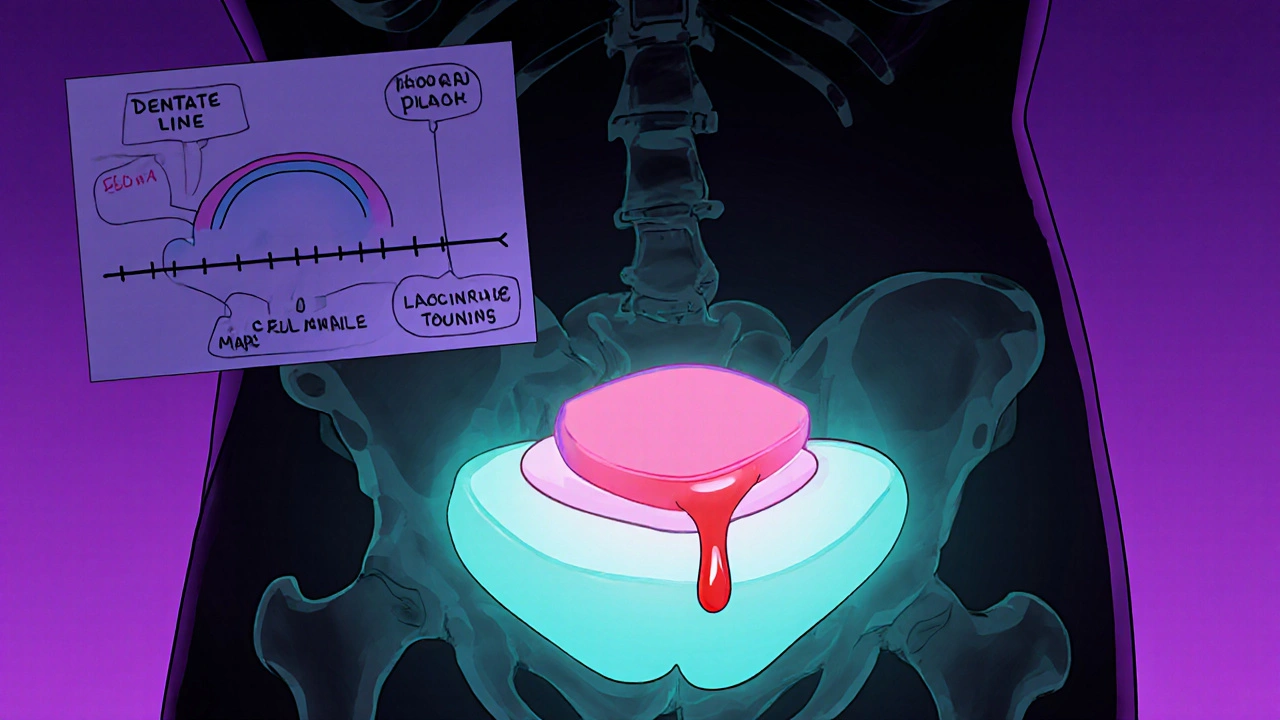
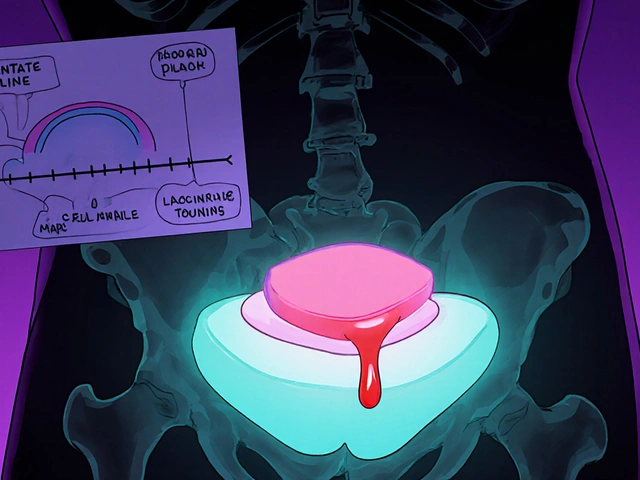
Internal hemorrhoids form inside the rectum, above a line called the dentate line. This area doesn’t have pain nerves, so even when they swell, you might not feel pain. That’s why they’re often called “silent.” But they do send other signals. The most common sign? Bright red blood. You’ll see it on your toilet paper after wiping, in the bowl, or streaked on your stool. It’s usually not mixed in with the stool-it sits on top. That’s a key difference from more serious conditions like colon cancer. Internal hemorrhoids are graded from I to IV based on how much they prolapse (protrude):- Grade I: Bleeds but doesn’t come out of the anus.
- Grade II: Pops out when you strain but slides back in on its own.
- Grade III: Comes out and stays out-you have to push it back in.
- Grade IV: Stays out permanently and can’t be pushed back.
External Hemorrhoids: The Painful Ones
External hemorrhoids form under the skin around the anus. This area is packed with pain nerves. So when they swell, you feel it-badly. You’ll notice a soft, skin-colored lump near your anus. It might itch, burn, or ache, especially when you sit. Sitting on a chair, driving, or even lying down can become uncomfortable. Worse yet? Thrombosed external hemorrhoids. This happens when a blood clot forms inside the swollen vein. The lump turns dark purple or blue, feels hard, and causes sudden, intense pain. It’s like a bruise that won’t go away. Many people describe it as the worst pain they’ve ever felt in that area. And here’s something most people don’t realize: You can have both internal and external hemorrhoids at the same time. That’s why symptoms can be confusing. One day you’re bleeding silently, the next you’re wincing every time you sit down.What Causes Hemorrhoids?
It’s not just “eating too little fiber.” While that’s part of it, the real culprits are repeated pressure on the veins in your lower rectum. Here’s what actually triggers them:- Chronic constipation or diarrhea-both make you strain.
- Sitting on the toilet for more than 5 minutes. Yes, scrolling on your phone while pooping counts.
- Pregnancy-the growing uterus presses on pelvic veins.
- Obesity-extra weight increases pressure everywhere.
- Heavy lifting-especially with poor form.
- Genetics-some people just have weaker vein walls.
How to Tell It’s Not Something Worse
This is critical: Rectal bleeding is never normal-even if you think it’s hemorrhoids. Other conditions like anal fissures, inflammatory bowel disease, or colorectal cancer can mimic hemorrhoid symptoms. Fissures cause sharp, tearing pain during bowel movements, often with a visible crack in the skin. Hemorrhoids cause more of a dull ache or itching. Fissures rarely cause lumps. Hemorrhoids do. If you’re over 50, have a family history of colon cancer, or notice changes in your bowel habits-like narrower stools, unexplained weight loss, or persistent fatigue-get checked. Don’t assume it’s hemorrhoids. A doctor can rule out the big stuff in minutes.Treatment: From Home Fixes to Surgery
You don’t need surgery right away. Most cases improve with simple changes.Step 1: Lifestyle Changes
- Eat 25-30 grams of fiber daily. That’s 1 cup of cooked lentils, 2 cups of broccoli, 1 pear, and a bowl of oatmeal. Fiber softens stool so you don’t strain.
- Drink 8-10 glasses of water. Fiber without water makes stool harder.
- Don’t sit on the toilet longer than 5 minutes. Use a small footstool to raise your knees above your hips. This straightens your rectum and cuts pressure by 30%.
- Move more. Walking 20-30 minutes a day helps everything.
Step 2: Over-the-Counter Relief
- Witch hazel pads: Soothe itching and swelling. Apply after each bowel movement.
- Hydrocortisone cream (1%): Reduces inflammation. Don’t use longer than 7 days.
- Sitz baths: Sit in warm (not hot) water for 15-20 minutes, 2-3 times a day. It reduces swelling and relaxes the muscles.
Step 3: Minimally Invasive Procedures
If home care doesn’t help after a few weeks, your doctor might suggest one of these:- Rubber band ligation: A tiny band is placed around the base of the internal hemorrhoid. It cuts off blood flow. The hemorrhoid shrivels and falls off in 5-7 days. It’s 90% effective for Grades I-III.
- Sclerotherapy: A chemical is injected into the hemorrhoid to shrink it.
- Infrared coagulation: Heat is applied to seal off the blood vessels.
Step 4: Surgery for Severe Cases
If you have Grade IV hemorrhoids, recurrent prolapse, or a thrombosed external hemorrhoid that won’t quit, surgery might be needed.- Hemorrhoidectomy: The hemorrhoid is completely removed. It’s the most effective-95% success rate-but recovery takes 2-4 weeks. Pain is real, and you’ll need prescription pain meds.
- Stapled hemorrhoidopexy: The tissue is lifted back into place and stapled. Less pain than removal, but higher chance of recurrence.
- Thrombectomy: For a fresh thrombosed external hemorrhoid (within 72 hours), a small cut is made to remove the clot. Instant pain relief.
What Doesn’t Work (And Why)
There’s a flood of “miracle cures” online: herbal ointments, tea tree oil, essential oils, hemorrhoid pills you order from a website with a .xyz domain. None of these are backed by science. The American Gastroenterological Association warns against them. They don’t fix the underlying issue. At best, they mask symptoms. At worst, they delay real treatment and let things get worse.
When to See a Doctor
Don’t wait. See a doctor if:- Bleeding lasts more than a week or gets worse.
- Pain is severe and doesn’t improve with home care.
- You feel dizzy, weak, or short of breath-signs of blood loss.
- Your stool is black, tarry, or mixed with blood.
- You’ve had changes in bowel habits for more than a few weeks.
Preventing Recurrence
The biggest mistake people make? Treating the symptoms, then going back to the same habits. Studies show that people who stick to high-fiber diets and proper toilet habits have only a 5-10% chance of hemorrhoids coming back. Those who don’t? Up to 50%. Keep eating fiber. Drink water. Don’t sit on the toilet scrolling. Move every hour if you work at a desk. If you’re pregnant, do pelvic floor exercises. It’s not glamorous-but it works.Final Thought
Hemorrhoids are embarrassing, but they’re not rare. They’re not a sign you did something wrong. They’re a sign your body’s under pressure-and it’s asking for help. You don’t need to suffer quietly. You don’t need to buy unproven products. You just need to make a few smart changes and, if needed, get the right treatment. Millions of people live pain-free after this. So can you.Can internal hemorrhoids turn into external ones?
No, internal and external hemorrhoids form in different areas and have different tissue types. But an internal hemorrhoid can prolapse-push out through the anus-and then become irritated or swollen like an external one. It’s still the same hemorrhoid, just in a different position. It doesn’t change type.
Is it safe to pop a thrombosed hemorrhoid at home?
Absolutely not. Trying to pop or cut a thrombosed hemorrhoid yourself can cause serious infection, bleeding, or scarring. If it’s very painful and recent (within 72 hours), see a doctor. They can safely drain it with a tiny incision under local anesthesia. After that, it heals much faster.
Do hemorrhoids go away on their own?
Mild hemorrhoids often improve within a few days with home care-especially if you fix your diet and bowel habits. But they rarely disappear completely unless the root cause (like straining or sitting too long) is addressed. Without lifestyle changes, they come back.
Can hemorrhoids cause cancer?
No, hemorrhoids do not cause cancer. But rectal bleeding-whether from hemorrhoids or something else-can be a sign of colorectal cancer. That’s why any new or persistent bleeding needs to be checked by a doctor. Don’t assume it’s just hemorrhoids, especially if you’re over 50 or have other risk factors.
Are hemorrhoids more common in men or women?
They affect men and women equally overall. But women are more likely to develop them during pregnancy, especially in the third trimester. Men are more likely to develop them due to heavy lifting or prolonged sitting at work. So the causes differ, but the rates are similar.
Can I exercise with hemorrhoids?
Yes-especially walking, swimming, and cycling. Avoid heavy weightlifting or exercises that involve straining (like intense core workouts or squats with heavy weights). Exercise helps prevent constipation and improves circulation, which reduces pressure on rectal veins. Just don’t push through pain.
Man I used to think hemorrhoids were just a myth people made up to scare kids into eating veggies
So I’ve been ignoring this for months and now I’m scared to poop. Like… what if it’s not hemorrhoids? What if it’s something worse? I’m gonna go see a doctor tomorrow. I can’t keep living like this.
It’s funny how society treats hemorrhoids like a moral failing. Like if you have them, you’re lazy, you eat too much junk, you don’t ‘take care of yourself.’ But the truth? Your body is a biological machine under pressure. It’s not about willpower. It’s about anatomy, gravity, and the brutal reality of modern life. We sit too much. We strain too often. We ignore our bodies until they scream. And then we shame the scream.
There’s no virtue in suffering silently. There’s no honor in ignoring your own biology. The real sin isn’t having hemorrhoids-it’s pretending they’re a personal failure instead of a systemic one.
And don’t even get me started on those ‘miracle cures’ online. People will buy snake oil from a guy named ‘Dr. Bubba’ on a .xyz site but won’t spend $10 on a footstool. We’ve outsourced common sense to algorithms and influencers. We’d rather believe in magic than fix our posture.
It’s not about fiber. It’s about how we live. We’re not designed to sit for 10 hours straight. We’re not designed to scroll while we poop. We’re not designed to treat our bodies like disposable machines.
So yeah, hemorrhoids are common. But the culture that lets them fester? That’s the real disease.
Oh my god I just realized I’ve been sitting on the toilet for 20 minutes every morning scrolling through TikTok. I thought I was ‘relaxing’ but I was basically giving my rectum a daily torture session. I’m getting a footstool today. And I’m deleting my bathroom apps. No more doomscrolling on the porcelain throne. I’m not a human toilet. I’m a person.
lol why so serious? just use some witch hazel and chill. its not cancer bro. just a little blood. happens to everyone. dont be a drama queen
Most of you are missing the point entirely. This isn’t about hemorrhoids. This is about the collapse of bodily autonomy in a capitalist society. We’re told to ‘fix’ ourselves with OTC creams while corporations profit from our discomfort. We’re sold fiber supplements while our jobs demand we sit for 12 hours. We’re shamed for needing surgery while insurance denies coverage. Hemorrhoids are the symptom. The disease is late-stage capitalism.
And don’t get me started on ‘lifestyle changes.’ Who has time to eat 30 grams of fiber when you’re working two jobs and your landlord raised the rent again? This isn’t self-help. It’s structural violence dressed up as wellness advice.
you guys are overthinking this. i had a thrombosed one last year. doc popped it in 5 mins. no big deal. just dont be a baby. also stop using the word ‘prolapse’ like its a bad thing. its just anatomy. you dont need to sound like a med student to talk about your butt
I’ve been dealing with this for years and I just want to say… thank you for writing this. I’ve felt so alone in this. Like no one understands how exhausting it is to plan your whole day around a bowel movement. I’ve canceled plans. I’ve cried in the bathroom. I’ve Googled ‘is this cancer’ at 3 a.m. And then I read this and I realized-I’m not broken. My body just needs a little more care. And that’s okay.
Why do Americans always make everything a health crisis?? I’m from the old country-we just ate spicy food, sat on the floor, and didn’t complain. You sit on a throne and cry because your butt hurts? We had 10 kids, no toilet paper, and still walked 5 miles to work. You’re weak. And you’re making hemorrhoids a culture war.
Also, why are you all so obsessed with fiber? Eat rice. Eat beans. Stop buying expensive ‘superfoods.’ Your great-grandparents didn’t know what ‘prebiotic’ meant and they lived to 90.
I really appreciate how detailed this is. I’ve been trying to figure out if I have internal or external and I kept confusing the symptoms. The grading system was super helpful-now I know mine is Grade II. I’ve started the footstool thing and I swear, it’s already better. Also, I’m drinking more water. I know it sounds basic, but it’s working. Thank you for not making me feel stupid for asking.
I’ve been reading all these comments and I just want to say-no one here is wrong. Some people need surgery. Some need fiber. Some need to stop sitting so much. Some need therapy for their toilet shame. We’re all at different places. There’s no one-size-fits-all. Just be kind to yourself and to each other.
From India to America-this issue is universal. In my village, we used to sit on the ground and squat. No chairs. No toilet paper. Just water and a bucket. No hemorrhoids. No problems. But now everyone sits on seats, eats junk, and blames their body. The solution is simple: return to natural posture. No magic creams. No pills. Just squat.
Try it. You’ll be surprised.
As someone who grew up in a culture where discussing bodily functions was taboo, I’m grateful this post exists. In my family, we never talked about hemorrhoids. My grandmother had them for 40 years and never saw a doctor. She suffered in silence. I’m breaking that cycle. I’m going to the doctor. And I’m telling my kids it’s okay to talk about their bodies. No shame. No silence.
While the information provided is comprehensive and clinically accurate, I would respectfully suggest that the author consider citing peer-reviewed sources to further validate the 90% and 95% efficacy claims for rubber band ligation and hemorrhoidectomy. Additionally, the distinction between ‘internal hemorrhoids prolapsing’ and ‘becoming external’ warrants clarification in medical literature, as the tissue composition remains unchanged regardless of position. A reference to the American Society of Colon and Rectal Surgeons guidelines would enhance the credibility of the piece.