GERD Chest Pain Assessment Tool
This tool helps you determine if your chest pain is more likely related to GERD or a heart issue based on the characteristics of your symptoms. For life-threatening symptoms, always call emergency services immediately.
Your Symptoms
Call 911 or emergency services immediately if you experience any of these symptoms:
- Sudden severe chest pain lasting longer than 15 minutes
- Chest pain with shortness of breath, sweating, or fainting
- Pain that radiates to left arm, jaw, or back and doesn't ease with antacids
- New chest pain after a traumatic injury
Ever felt a burning squeeze behind your breastbone and wondered if your heart was under attack? That tight, unsettling feeling could be your heart, but it could also be a classic case of GERD chest pain. Understanding how gastroesophageal reflux disease (GERD) triggers chest discomfort helps you avoid panic, get the right treatment, and know when a trip to the emergency room is truly necessary.
What Is Gastroesophageal Reflux Disease (GERD)?
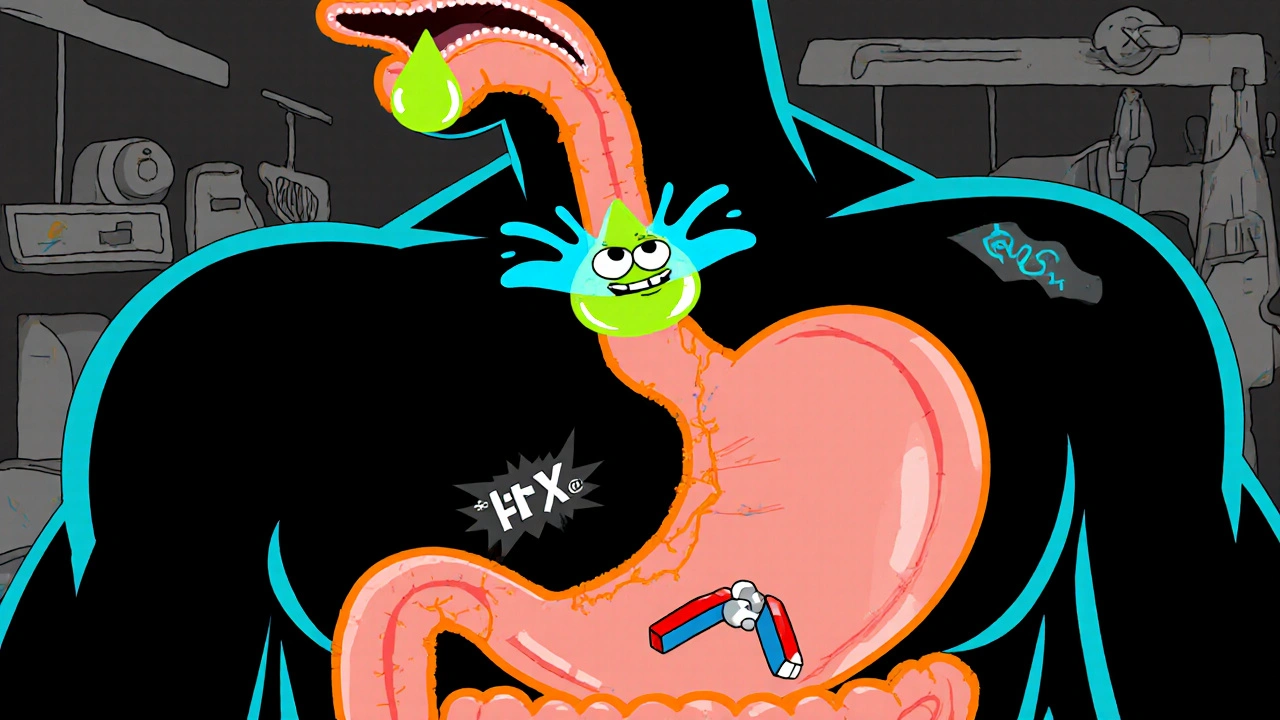
When you hear the term Gastroesophageal Reflux Disease (GERD) is a chronic condition where stomach acid repeatedly backs up into the esophagus, causing irritation and inflammation, think of a faulty valve that can’t keep the stomach’s contents where they belong. Most people experience occasional heartburn, but GERD is defined by symptoms that occur at least twice a week or cause complications like esophagitis.
The culprit is the Lower Esophageal Sphincter (LES), a ring of muscle at the bottom of the Esophagus. When the LES relaxes inappropriately or weakens, acid slips upward, burning the esophageal lining and sometimes spilling over into the chest cavity.
How GERD Can Lead to Chest Pain
There are three main ways GERD creates chest discomfort:
- Acid irritation: Direct contact of stomach acid with the esophageal mucosa triggers pain receptors that transmit signals to the chest area.
- Esophageal spasm: Acid can cause the esophagus to contract erratically, mimicking the cramping you might feel during a heart attack.
- Hiatal hernia involvement: A Hiatal Hernia pushes part of the stomach up through the diaphragm, increasing reflux episodes and intensifying chest pain.
Because the esophagus and heart share nerve pathways (the vagus nerve), the brain can misinterpret esophageal pain as cardiac pain-a phenomenon known as "referred pain."
GERD Chest Pain vs. Cardiac Chest Pain: Spot the Differences
Distinguishing reflux‑related pain from a heart problem can be tricky, but certain patterns help. Below is a quick side‑by‑side comparison.
| Feature | GERD‑Related Chest Pain | Cardiac Chest Pain (Angina/Heart Attack) |
|---|---|---|
| Typical Trigger | After large meals, lying down, spicy/fatty foods, caffeine, alcohol | Physical exertion, emotional stress, cold weather |
| Pain Quality | Burning, pressure, or a “tight” feeling that may radiate to the throat | Heavy pressure, squeezing, or crushing sensation, often radiating to left arm, jaw, or back |
| Duration | Minutes to several hours; often improves with antacids or sitting up | Typically 5‑30 minutes; does not improve with antacids, may worsen with activity |
| Associated Symptoms | Regurgitation, sour taste, hoarseness, chronic cough | Shortness of breath, sweating, nausea, dizziness |
| Response to Relief Measures | Improves with upright posture, chewing gum, proton pump inhibitors | Requires medical attention; nitroglycerin may help in angina |
If you’re ever unsure, treat it as a cardiac emergency until proven otherwise.
Red‑Flag Symptoms: When to Call 911
Even if you suspect GERD, certain signs demand immediate medical help:
- Sudden, severe chest pain lasting longer than 15 minutes
- Chest pain accompanied by shortness of breath, sweating, or fainting
- Pain that radiates to the left arm, jaw, or back and does not ease with antacids
- New onset of pain after a traumatic injury to the chest
- Persistent vomiting, black stools, or signs of bleeding
When in doubt, dial emergency services. It’s better to be safe than to miss a heart attack.
Managing GERD‑Related Chest Pain
Most people can control reflux‑induced chest discomfort with a combination of lifestyle tweaks, over‑the‑counter meds, and, when needed, prescription therapy.
1. Lifestyle Modifications
Adopt these daily habits to keep acid at bay:
- Eat smaller meals < 3‑4 hours before bedtime.
- Elevate the head of your bed by 6‑8 inches.
- Avoid trigger foods: citrus, tomato‑based sauces, chocolate, mint, fried foods, and carbonated drinks.
- Quit smoking - nicotine relaxes the LES.
- Maintain a healthy weight; excess abdominal pressure worsens reflux.
- Practice stress‑reduction techniques (deep breathing, yoga) since stress can exacerbate LES relaxation.
2. Over‑the‑Counter Options
Try these first‑line agents for short‑term relief:
- Antacids (Tums, Maalox) neutralize existing acid quickly.
- H2 blockers (ranitidine, famotidine) reduce acid production for up to 12 hours.
- Proton Pump Inhibitors (PPIs) - see next section.
3. Prescription‑Strength PPIs
Proton Pump Inhibitors (PPIs) like omeprazole, esomeprazole, and lansoprazole are the gold standard for chronic GERD. They block the final step of acid secretion, offering 24‑hour relief and promoting healing of Esophagitis (inflammation of the esophagus). Typical courses last 4‑8 weeks, after which a doctor may taper the dose.
Watch the dose: long‑term PPI use can increase risk of nutrient malabsorption (B12, magnesium) and infections, so follow up with your physician regularly.
4. When Surgery Is Considered
About 10‑15 % of GERD patients don’t respond to medication. Surgical options include:
- Fundoplication - wrapping the top of the stomach around the LES to reinforce the valve.
- LINX device - a ring of magnetic beads placed around the LES to keep it closed yet allow food passage.
Both procedures aim to stop reflux and, consequently, eliminate chest pain without lifelong drugs.

Common Myths About GERD and Chest Pain
Myth #1: "If I have chest pain, it’s always my heart." - Not true. Up to 30 % of emergency‑room chest pain cases are later diagnosed as non‑cardiac, mostly GERD.
Myth #2: "Antacids cure GERD forever." - Antacids only neutralize acid temporarily; they don’t heal the LES or prevent future episodes.
Myth #3: "Spicy food always triggers GERD." - While many report discomfort after spicy meals, the main culprits are high‑fat foods and large portions, not just heat.
Myth #4: "Stress only affects the mind, not the gut." - Stress releases cortisol, which can relax the LES and increase acid production, directly worsening GERD.
Quick Checklist: Your Daily GERD‑Chest‑Pain Action Plan
- ⦿ Keep a food‑trigger diary for two weeks.
- ⦿ Eat meals no larger than a fist‑size portion.
- ⦿ Wait at least 3 hours after dinner before lying down.
- ⦿ Use a wedge pillow or elevate the bed head.
- ⦿ Take a daily PPI if prescribed, with the first dose before breakfast.
- ⦿ Schedule a follow‑up endoscopy if symptoms persist >8 weeks.
Frequently Asked Questions
Can GERD cause a heart attack?
No. GERD doesn’t damage the heart. However, its chest pain can mimic heart attack symptoms, which is why doctors often run cardiac tests to rule out a true heart event.
How long does GERD‑related chest pain usually last?
It can last from a few minutes to several hours. Relief typically follows an upright position, antacids, or a PPI dose.
Is it safe to take antacids every day?
Occasional use is fine, but daily antacid use may mask underlying problems and lead to electrolyte imbalances. Talk to a doctor about a long‑term plan.
What is non‑cardiac chest pain (NCCP)?
NCCP describes chest discomfort that isn’t caused by heart disease. GERD, esophageal spasm, anxiety, and musculoskeletal issues are common sources.
Can I exercise if I have GERD‑related chest pain?
Yes, but choose low‑impact activities (walking, cycling) and avoid vigorous workouts right after meals. If pain spikes during exercise, stop and consult a doctor.
When should I see a gastroenterologist?
If over‑the‑counter meds and lifestyle changes don’t reduce chest pain within 8‑12 weeks, or if you develop difficulty swallowing, weight loss, or frequent vomiting, schedule a specialist appointment.
Do PPIs have side effects?
Long‑term use can lower magnesium, calcium, and vitamin B12 levels, and may increase risk of certain infections. Short courses are generally safe; discuss monitoring with your doctor.
Understanding the link between GERD and chest pain empowers you to act confidently-whether that means adjusting your diet, starting a medication, or calling emergency services. Keep this guide handy, and you’ll know exactly what to do the next time that tightness hits.


I’ve found keeping a food diary makes a big difference.
Tracking what you eat and when you lie down can reveal hidden triggers. Many people don’t realize that even a small snack before bed can cause reflux. I try to eat a light dinner at least three hours before sleeping and it’s helped my chest tightness. The simple habit of noting symptoms also guides the doctor.
GERD isn’t an excuse for neglecting heart health; people must rule out cardiac issues first.
It’s easy to feel anxious when that pressure hits out of nowhere. Remember that lifestyle tweaks-like raising the head of the bed-can reduce acid backflow. If you’re still unsure, a quick check‑up can give peace of mind. You deserve both comfort and certainty.
Elevating your pillow and skipping coffee after dinner are cheap fixes that often get overlooked.
Good points, especially the timing of meals; I also add a short walk after dinner to aid digestion.
That pressure can be scary, but knowing the difference between reflux and heart pain is empowering. Staying hydrated with water rather than soda helps keep the esophagus calm. If you ever feel the pain linger despite antacids, check in with a doctor.
When you’re dealing with GERD‑related chest pain, think of it as a marathon, not a sprint. First, identify your personal trigger foods and keep a simple log; the act of writing things down often makes patterns obvious. Second, experiment with portion sizes-smaller meals reduce stomach pressure and give the LES a better chance to stay closed. Third, the position you sleep in matters; a wedge pillow or raising the bed head 6‑8 inches can keep acid where it belongs. Fourth, avoid lying down within three hours of eating, and try to stay upright after meals, even a short walk can be beneficial. Fifth, nicotine is a known LES relaxant, so quitting smoking can dramatically improve symptoms. Sixth, if you’re overweight, even modest weight loss can lower intra‑abdominal pressure and lessen reflux episodes. Seventh, when over‑the‑counter meds aren’t enough, discuss a short course of PPIs with your physician; they’re effective but should be monitored. Eighth, be aware of long‑term PPI risks-magnesium and B12 deficiencies-and get labs checked periodically. Ninth, consider trying an H2 blocker at night if you notice symptoms waking you up. Tenth, hydration with plain water helps dilute stomach acid, but avoid carbonated drinks that can increase bloating. Eleventh, stress management techniques like deep breathing or yoga can calm the vagus nerve and reduce LES relaxation. Twelfth, keep an eye on extra‑esophageal symptoms like chronic cough or hoarseness-they often signal reflux. Thirteenth, if lifestyle and meds fail after a few months, ask about a gastroenterology referral for possible endoscopy. Fourteenth, surgical options such as fundoplication or LINX are reserved for refractory cases, but they can be life‑changing. Fifteenth, remember that occasional heartburn is normal; it’s the chronic, frequent episodes that warrant attention. Finally, always treat new, severe chest pain as a potential cardiac emergency until proven otherwise; calling 911 can save lives.
Totally agree; those low‑key tweaks are often the most effective, and they cost nothing.
While elevating the head of the bed can mitigate nocturnal reflux, it is essential to ensure the incline is consistent; an uneven surface may exacerbate discomfort.
Listen, the heart‑attack myth is dangerous, you can’t just assume every tight feeling is reflux, you need to act fast, get an EKG, and don’t waste time debating on the internet!
I’ve been there, the sudden squeeze in the chest makes you wonder if you’re having a heart attack. I started by noting when the pain occurs and what I ate. Over weeks I cut out coffee after noon and raised my bed. The pain frequency dropped significantly. Still, I schedule regular check‑ups to keep my heart health in check. Small steps add up, and you’re not alone in figuring this out.
While urgency is warranted in evaluating chest discomfort, it is equally important to differentiate cardiac ischemia from gastroesophageal etiologies through appropriate diagnostic testing, including ECG and possibly endoscopic evaluation, before arriving at a definitive conclusion.
Yo, if ur chest pain is like “acid reflux vibes” then dat’s just GERD, but don’t be lax, do a stress test and maybe a barium swallow to rule out hiatal hernia, ya know?
Excellent synthesis of practical recommendations; the stepwise approach you outlined aligns with evidence‑based guidelines and offers readers a clear roadmap to manage GERD‑related chest discomfort.