Imagine this: a patient with type 2 diabetes feels nauseous, tired, and has stomach pain. Their blood sugar is 180 mg/dL - not high enough to raise alarms. They’re told it’s just a stomach bug. Two days later, they collapse. This isn’t rare. It’s euglycemic diabetic ketoacidosis - a dangerous form of DKA that hides in plain sight because blood sugar stays normal. And it’s rising because of a class of diabetes drugs called SGLT2 inhibitors.
What Is Euglycemic DKA, and Why Does It Happen?
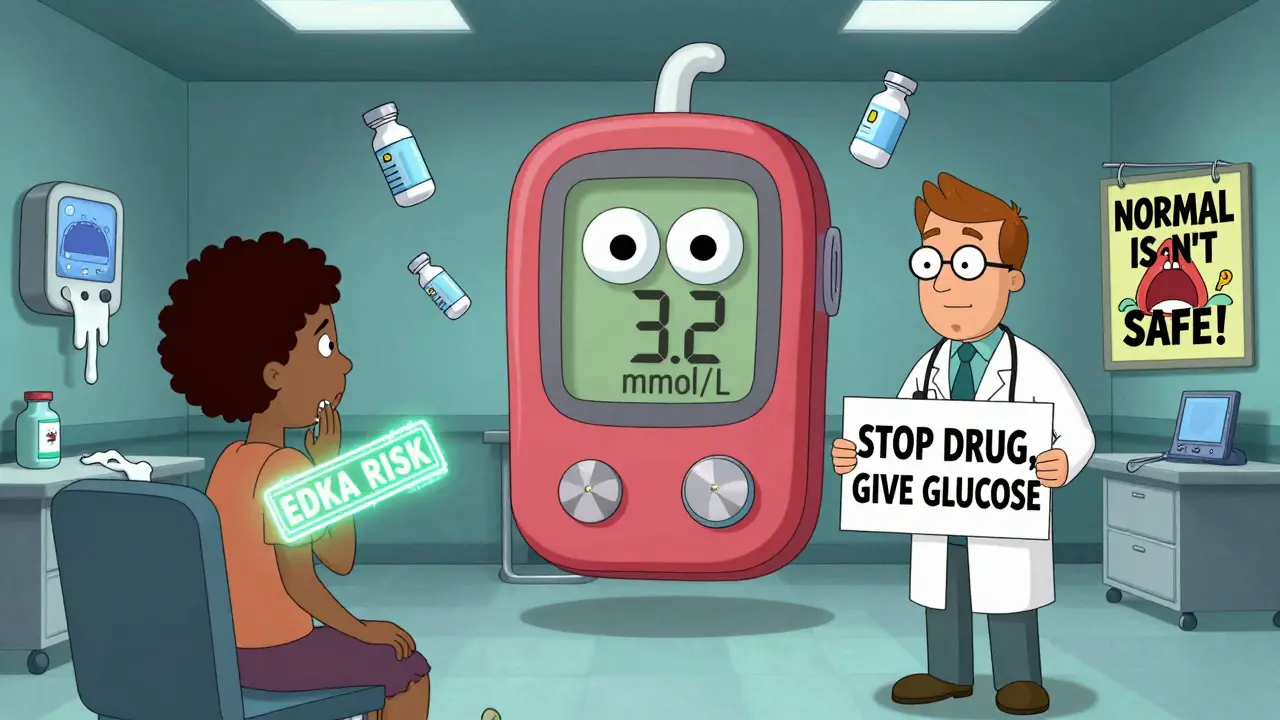
Euglycemic diabetic ketoacidosis (EDKA) is diabetic ketoacidosis without the high blood sugar you’d expect. Classic DKA happens when insulin drops, the body burns fat for fuel, and ketones flood the bloodstream - along with blood glucose over 250 mg/dL. EDKA looks the same: acidosis, ketones, nausea, rapid breathing - but glucose stays below 250 mg/dL. That’s the trap. It’s tied to SGLT2 inhibitors like dapagliflozin (Farxiga), empagliflozin (Jardiance), and canagliflozin (Invokana). These drugs work by making your kidneys dump glucose into urine. That lowers blood sugar - great for control. But it also tricks your body into thinking it’s starving. Your pancreas releases more glucagon, less insulin. Fat breaks down. Ketones rise. And because glucose is being flushed out, your blood sugar doesn’t spike. You get ketoacidosis without the warning sign. This isn’t just theory. A 2015 study in Diabetes Care found 13 cases of EDKA linked to SGLT2 inhibitors in just nine patients. The FDA issued a warning that same year. Since then, data shows SGLT2 inhibitor users have a 7-fold higher risk of DKA than non-users. Even more alarming: 20% of EDKA cases happen in people with type 2 diabetes who’ve never had DKA before.Who’s at Risk?
Not everyone on these drugs gets EDKA. But certain situations make it far more likely:- Illness - colds, flu, infections
- Reduced food intake - skipping meals, fasting, dieting
- Surgery or trauma
- Pregnancy
- Alcohol use
- Insulin dose reduction (especially in type 1 diabetes)
How to Spot It - The Symptoms Are the Same
EDKA doesn’t have unique symptoms. It mimics every other common illness:- Nausea (85% of cases)
- Vomiting (78%)
- Abdominal pain (65%)
- Unusual fatigue (76%)
- Malaise (91%)
- Deep, fast breathing (Kussmaul respirations - 62%)

Lab Tests That Reveal the Truth
If you suspect EDKA, don’t wait for high glucose. Test for ketones - and test them right.- Blood beta-hydroxybutyrate: The gold standard. Levels above 3 mmol/L confirm ketoacidosis.
- Arterial blood gas: pH below 7.3, bicarbonate under 18 mEq/L = metabolic acidosis.
- Anion gap: Usually over 12 mEq/L.
- Serum glucose: Below 250 mg/dL - this is the red herring.
- Electrolytes: Potassium may look normal, but total body potassium is often dangerously low.
Emergency Treatment - It’s Different From Regular DKA
Treatment follows the same principles as classic DKA: fluids, insulin, electrolytes. But EDKA needs adjustments.- Fluids: Start with 0.9% saline at 15-20 mL/kg in the first hour. Dehydration is real. But don’t overdo it - you’re not dealing with severe hyperglycemia.
- Insulin: Begin at 0.1 units/kg/hour. But here’s the key: once glucose drops below 200 mg/dL, switch to 5% dextrose in saline. You can’t let glucose crash. The body’s already low on fuel.
- Potassium: Almost everyone needs replacement. Even if serum potassium is normal, total body stores are depleted. Start IV potassium early.
- Monitor closely: Check glucose every hour. Ketones every 2-4 hours. Electrolytes every 4-6 hours.
Prevention Is the Best Strategy
The FDA now requires SGLT2 inhibitor packaging to include this warning: "Stop taking this medication and seek medical help immediately if you have symptoms of ketoacidosis, even if your blood sugar is normal." Patients need clear instructions:- Stop your SGLT2 inhibitor during illness, surgery, or fasting.
- Check ketones if you feel unwell - even if your glucose is 150 or 200.
- Don’t skip meals. Eat carbohydrates even if you’re sick.
- Keep a blood ketone meter at home if you’re high-risk.
- Tell every doctor you see that you’re on an SGLT2 inhibitor.
Why This Matters Now
As of 2023, SGLT2 inhibitors make up 25% of all new diabetes prescriptions in the U.S. Dapagliflozin and empagliflozin are the most common. These drugs reduce heart failure and kidney disease - huge wins. But EDKA kills. And it kills quietly. Since 2015, awareness has cut overall DKA cases by 32%. But EDKA now makes up 41% of all SGLT2-related DKA - up from 28%. That means we’re getting better at spotting it, but the risk hasn’t gone away. It’s just more hidden. Research is moving fast. A study at 15 U.S. centers is testing a tool that predicts EDKA risk using HbA1c variability and C-peptide levels. Early results show 82% accuracy. That could one day tell you if you’re in danger before you even feel sick. But right now, the only tool that saves lives is knowledge. If you’re on an SGLT2 inhibitor, you must know: normal glucose does not mean safe. Ketones don’t care about your blood sugar number. They care about insulin, glucagon, and fuel.Frequently Asked Questions
Can you get euglycemic DKA if you have type 2 diabetes?
Yes. While most people associate DKA with type 1 diabetes, about 20% of EDKA cases occur in people with type 2 diabetes who’ve never had ketoacidosis before. SGLT2 inhibitors can trigger it even in those with some insulin production, especially during illness or low food intake.
Should I stop taking my SGLT2 inhibitor if I’m sick?
Yes - temporarily. If you have an infection, vomiting, diarrhea, or are fasting for surgery, stop your SGLT2 inhibitor until you’re well. Talk to your doctor about when to restart. Never ignore nausea or fatigue while on these drugs.
Is urine ketone testing enough to rule out EDKA?
No. Urine strips can be normal even when blood ketones are high, especially if you’re well-hydrated. Blood beta-hydroxybutyrate testing is the only reliable way to diagnose ketoacidosis in this context. Always use a blood ketone meter if you suspect EDKA.
Why do I need glucose in my IV fluids if my blood sugar is normal?
Because insulin therapy rapidly lowers ketones - but it also lowers blood sugar fast. If you’re already euglycemic, giving insulin without glucose can cause dangerous hypoglycemia. Adding 5% dextrose to IV fluids keeps your glucose stable while treating the acidosis.
Are SGLT2 inhibitors still safe to use?
Yes - if used correctly. These drugs reduce heart failure, kidney damage, and death in high-risk patients. The risk of EDKA is low - about 0.16 to 0.76 events per 1,000 patient-years. But it’s preventable. Know the signs. Check ketones when sick. Stop the drug during stress. Talk to your doctor. Don’t let fear stop you - but don’t ignore the warning.


Wow. I’m on Farxiga and just had a weird bout of nausea last week - thought it was just bad sushi. Now I’m checking my ketones with my meter. Scary how normal glucose can lie like that.
Oh great. So now instead of just dying from diabetes, we get to die from *fancy* diabetes. SGLT2 inhibitors: because why treat the disease when you can invent a new way to die in a hospital gown?
EDKA is just a metabolic decompensation cascade triggered by SGLT2i-mediated glucagon dysregulation and suppressed insulin secretion under caloric stress. The anion gap’s your friend. Ketones >3 mmol/L = non-negotiable. Stop relying on glucose. It’s a decoy.
so like... if my sugar is normal but i feel like i'm gonna die... i should just assume it's ketoacidosis?? nope. nope nope nope. i'm not falling for that one. i'm gonna keep drinking my diet coke and hope for the best
THIS IS A MASSACRE. WHY ISN’T EVERYONE TALKING ABOUT THIS?! MY COUSIN ALMOST DIED BECAUSE THE ER DOCTOR SAID ‘IT’S JUST A STOMACH BUG’ - AND SHE WAS ON JARDIANCE! DOCTORS AREN’T TRAINED FOR THIS. PHARMACIES DON’T WARN PEOPLE. THIS IS A CRIME.
Let’s step back for a second and ask ourselves: what does it mean to be ‘normal’ in a body that’s been chemically reconfigured by pharmaceutical ambition? The glucose reading isn’t a lie - it’s a performance. A stage trick. The body is screaming in ketones, but the machine says ‘all clear’ because the algorithm was designed for simplicity, not survival. We’ve outsourced our intuition to lab results, and now we’re paying for it in ICU beds. Is this medicine - or is this capitalism dressed in white coats? The SGLT2 inhibitors didn’t create this crisis. They just exposed how deeply we’ve forgotten how to listen to the body when it speaks in silence.
Just checked my ketones after a cold. 1.2 mmol/L. Not high. But I stopped the drug anyway. Better safe than sorry. Docs don’t always know. You gotta be your own advocate.
in Nigeria we don’t have ketone meters. we just know when someone is breathing weird and looks pale. if you on this medicine and feel sick - go to hospital. don’t wait. your sugar can be fine but your body is breaking.
Thank you for writing this. 🙏 I’m a nurse and we’ve had two EDKA cases this year - both missed at first. I’ve started keeping ketone strips in my desk now. Everyone on SGLT2s gets a handout. Small steps, but they matter. 💙
One thing I learned from my endo: if you’re on an SGLT2i and you’re sick, treat it like you’re diabetic type 1 - even if you’re not. That mindset shift saved me last winter. No more ‘it’s just a bug’.
So let me get this straight - we’re supposed to stop a drug that keeps my heart and kidneys healthy just because it might cause a rare but deadly side effect? And then we’re supposed to buy a blood ketone meter? That’s like saying ‘don’t drive because you might get into a crash’. The risk is real, but the benefit is massive. Just be smart. Don’t panic. Check ketones when sick. Stop the drug. Eat carbs. Talk to your doctor. That’s not hard.