A cerebral aneurysm isn’t something you hear about until it’s too late. Most people live with one for years without knowing. But when it ruptures, the consequences are sudden, brutal, and often fatal. About cerebral aneurysm ruptures happen every year in the UK alone, and nearly half of those cases end in death within the first day. The scary part? Many of these could have been caught and treated before they burst.
What Exactly Is a Cerebral Aneurysm?
A cerebral aneurysm is a weak spot in the wall of a brain artery that balloons out like a tiny bubble. Think of it like a bulge in an old garden hose - the pressure from blood flow keeps pushing against the thin spot. Most are small, under 7 mm, and stay harmless. But some grow, change shape, or get stressed by high blood pressure - and then they burst.
It’s not a tumor. It’s not cancer. It’s a structural flaw in a blood vessel. And once it ruptures, it bleeds into the space around the brain - called a subarachnoid hemorrhage. That’s what causes the sudden, worst-headache-of-your-life pain, vomiting, confusion, or even collapse.
Who’s at Risk?
Some risks you can’t change. Age is one. If you’re over 65, your chance of rupture is more than double that of someone in their 40s. Women are 1.6 times more likely than men to develop one, especially after menopause. And if two or more close family members have had an aneurysm, your risk jumps fourfold.
But the biggest dangers? The ones you can control.
High blood pressure - especially systolic readings above 140 - makes rupture 2.3 times more likely. Smoking? That’s even worse. Current smokers face a 3.1-fold higher risk. And it’s not just smoking - the more you smoke, the higher the danger. People who smoke 10 or more cigarettes a day see their risk rise by nearly 50%. Heavy drinking - more than 14 drinks a week - adds another 32% risk.
And here’s something most people don’t realize: having more than one aneurysm doesn’t just double your risk. It triples it. If you’ve had one rupture before, your chance of another is over five times higher.
What Makes an Aneurysm More Likely to Burst?
Size matters - but not in the way you think. Aneurysms larger than 7 mm have a 3.1 times higher chance of rupturing than smaller ones. But some tiny ones burst anyway. Location is just as important. Aneurysms at the front of the brain, especially near the anterior communicating artery (AComm), rupture more often - even if they’re under 5 mm. These are the silent killers.
Shape is another clue. Aneurysms with irregular edges, lobes, or daughter sacs (small bumps growing off the main bulge) are far more unstable. They carry a 2.9 times higher rupture risk than smooth, round ones.
Inside the blood vessel, blood flow plays a hidden role. Areas with chaotic, swirling, or low-pressure flow - called low wall shear stress - are where aneurysms are most likely to rupture. This isn’t guesswork. Computer models show 83% of ruptured aneurysms had these flow patterns, compared to just 42% of unruptured ones.
And biology? Inflammation is a big player. People whose aneurysms rupture have higher levels of IL-6 and CRP - markers of body-wide inflammation. Genetic changes in collagen and other structural proteins also make some people’s blood vessels more fragile.
How Do Doctors Predict the Risk?
There’s no single test that says, “This one will burst tomorrow.” But doctors use scores - tools built from data on thousands of patients - to estimate risk over time.
The PHASES score is the most trusted. It looks at six things: your population (ethnicity and region), blood pressure, age, aneurysm size, whether you’ve had a previous bleed, and where the aneurysm is located. Each factor adds points. A score of 0-3 means a 3% chance of rupture in five years. A score of 9-10? That’s a 45% chance.
Another tool, the triple-S model, focuses on Size, Site, and Shape. It’s especially useful if your aneurysm has grown since the last scan. It can predict your risk over 6 months, 1 year, or 2 years - with good accuracy.
Doctors don’t just guess. They combine these scores with imaging. Annual MRA scans (a type of MRI) track growth. If an aneurysm grows even 1 mm in a year, that’s a red flag.
Treatment Options: Clipping, Coiling, and Flow Diversion
If your aneurysm is high-risk, you’ll likely be offered treatment. There are three main ways to fix it.
Surgical Clipping
This is the oldest method - dating back to 1937. A neurosurgeon opens the skull (craniotomy), finds the aneurysm, and places a tiny titanium clip across its neck. It’s like putting a clamp on a leaky pipe. This stops blood from entering the bulge completely.
Success rate? About 95% of aneurysms are fully sealed. And once clipped, the cure is permanent. But it’s invasive. Recovery takes weeks. There’s a 1.5% risk of death and a 4.7% chance of permanent side effects like weakness or speech problems.
Endovascular Coiling
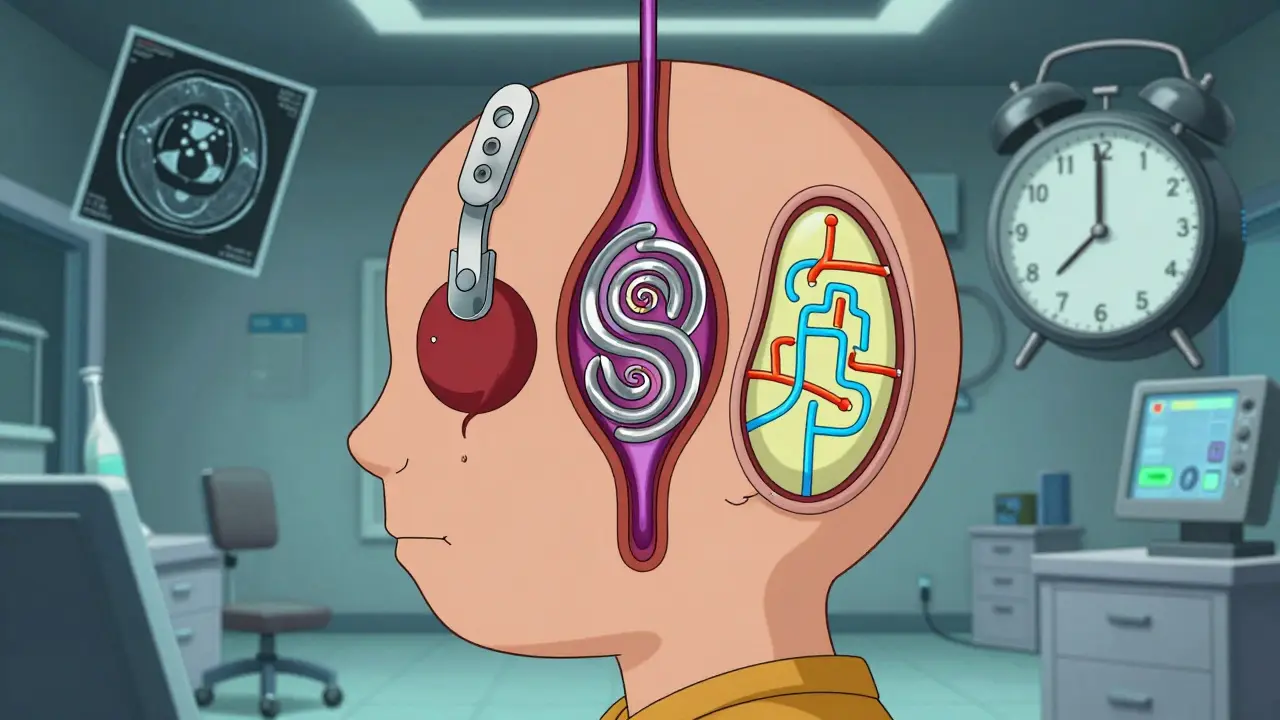
This is the less invasive option. A catheter is threaded from the groin up to the brain. Tiny platinum coils are pushed into the aneurysm. They fill the space, trigger clotting, and seal it off from the inside.
It’s quicker. Most patients go home in a day or two. The 1-year death rate is lower than clipping - 8.1% vs. 10.1% - according to the landmark ISAT trial. But there’s a catch: about 16% of coiled aneurysms need a second procedure later because they reopen.
Flow Diversion
This is the newest and most advanced. A stent-like device - like the Pipeline Embolization Device or WEB - is placed across the aneurysm’s opening. It doesn’t fill it. It redirects blood flow away from it. Over months, the aneurysm slowly shrinks and disappears.
It works best for large, wide-necked, or complex aneurysms that are hard to coil or clip. Success rates hit 85% after one year. Mortality is low - just 0.8%. But it requires long-term anti-clotting meds and carries a 5.2% risk of complications like stroke.
Which Treatment Is Right for You?
There’s no one-size-fits-all. Your doctor will weigh:
- Aneurysm size and shape: Large, irregular, or wide-necked? Flow diversion often wins.
- Location: Aneurysms in the back of the brain (posterior circulation) are riskier to clip - complications jump 22%.
- Your age: If you’re over 70, surgical risks go up 35%. Coiling or flow diversion are often preferred.
- Your health: High blood pressure, diabetes, or heart disease? That increases surgical risks by nearly 30%.
- Your PHASES score: If it’s 6 or higher, treatment is usually recommended. Below 6? Monitoring may be safer.
For small aneurysms under 5 mm in low-risk areas, many doctors just watch. The UCAS Japan study found the 5-year rupture risk for these was as low as 0.2%. Annual scans are enough.
What If You Don’t Treat It?
Leaving a high-risk aneurysm alone is dangerous. Without treatment, the 10-year re-rupture risk is 68%. That’s not a gamble - that’s a countdown.
But not every aneurysm needs fixing. Many people live with small, stable ones for life. The key is knowing which is which. That’s why imaging and scoring matter so much.

Medical Management: The Non-Surgical Shield
Even if you’re not having surgery, treatment starts with lifestyle. Quitting smoking cuts your rupture risk by 54% within two years. Controlling blood pressure to under 130/80 reduces strain on the vessel wall. Cutting back on alcohol helps too.
Medications like beta-blockers or calcium channel blockers may be used to lower blood pressure and reduce pulsatile stress on the aneurysm. No drug can make it disappear - but they can buy you time.
What’s Next? The Future of Treatment
Researchers are now looking at genetics. The HUNT study found 17 gene locations linked to aneurysm formation. In the future, a simple blood test might tell you if you’re genetically prone.
Machine learning is also stepping in. New AI models analyze hundreds of data points - shape, flow, wall thickness - to predict rupture better than current scores. One model, using 42 features, already outperforms PHASES in early testing.
New devices are coming too. The WEB device, approved in 2019, is already helping patients with aneurysms at artery branches - places that used to be nearly impossible to treat safely.
When to See a Doctor
You don’t need to panic if you have a headache. But if you suddenly feel the worst headache of your life - described as “like being hit by a hammer” - get help immediately. Other signs: sudden nausea, vision changes, stiff neck, or loss of consciousness.
If you have a family history of aneurysms, especially if two or more relatives had one, talk to your doctor about screening. MRA scans are non-invasive and safe.
And if you smoke? Quit. If your blood pressure is high? Get it under control. These aren’t just good habits - they’re life-saving actions.
Can a cerebral aneurysm go away on its own?
No, a cerebral aneurysm won’t disappear without treatment. In rare cases, a small aneurysm may form a clot and seal off naturally, but this is unpredictable and dangerous. Most remain active and can rupture at any time. Monitoring or medical intervention is always recommended for diagnosed aneurysms.
Are aneurysms hereditary?
Yes. If two or more first-degree relatives (parent, sibling, child) have had a cerebral aneurysm, your risk increases fourfold. Genetic factors affect blood vessel strength and inflammation response. Screening with MRA is strongly advised for people with this family history.
How often should I get scanned if I have an unruptured aneurysm?
For small, stable aneurysms under 7 mm with low PHASES scores, annual MRA scans are standard. If the aneurysm is growing, irregular, or larger, scans may be done every 6 months. Your neurologist will adjust based on your risk score, location, and changes in size or shape.
Can I exercise with a cerebral aneurysm?
Yes - but with limits. Avoid heavy lifting, intense straining, or high-impact sports that spike blood pressure. Walking, swimming, cycling at a moderate pace, and yoga are generally safe. Always check with your neurologist before starting any new routine. Sudden pressure spikes can trigger rupture in vulnerable aneurysms.
What’s the difference between coiling and clipping?
Clipping is open brain surgery - a surgeon places a metal clip on the aneurysm’s neck. Coiling is minimally invasive - a catheter delivers coils through the leg artery to fill the aneurysm. Clipping has a higher long-term success rate and lower retreatment risk, but longer recovery. Coiling has faster recovery and lower early death risk, but higher chance of needing another procedure later.
Is flow diversion better than coiling?
It depends on the aneurysm. Flow diversion works best for large, wide-necked, or complex aneurysms that coiling can’t fully treat. It has higher long-term occlusion rates (up to 85%) and lower retreatment needs. But it requires taking blood thinners for months and carries a slightly higher risk of delayed stroke. For smaller, simpler aneurysms, coiling is often still preferred.
Final Thoughts
A cerebral aneurysm isn’t a death sentence. It’s a condition you can manage - if you know the risks and act early. The tools to detect and treat it are better than ever. The key is awareness, screening when needed, and making smart lifestyle choices. Don’t wait for a headache to be your wake-up call.