Handling chemotherapy drugs isn’t just about giving the right dose at the right time. It’s about protecting lives-patients’, nurses’, pharmacists’, and even caregivers’-from toxic exposure that can cause cancer, infertility, or organ damage. The stakes are high, and the rules have changed. The latest chemotherapy safety standards, updated in 2024 by ASCO and the Oncology Nursing Society, aren’t suggestions. They’re mandatory. And if you’re not following them, you’re putting people at risk.
Why Chemotherapy Is Different From Other Medications
Most drugs are safe to handle with bare hands. Chemotherapy isn’t. Antineoplastic agents are designed to kill rapidly dividing cells. That’s why they work against cancer. But they don’t know the difference between a cancer cell and a healthy one-like those in your bone marrow, skin, or reproductive organs. Even tiny amounts of exposure over time can lead to serious health problems for healthcare workers. Studies dating back to 1992 show that contamination transfers from gloves to skin, then to surfaces, then to other people. One nurse touching a vial, then a doorknob, then a patient’s chart can spread traces of a drug without ever realizing it. The 2024 ASCO/ONS guidelines now call these drugs antineoplastic therapy, not just chemotherapy. That’s because modern cancer treatment includes targeted therapies, immunotherapies, and antibody-drug conjugates-all of which carry similar risks. Carmustine and thiotepa? They’re so potent they require double gloving. Others may need special ventilation or closed-system transfer devices. You can’t treat them all the same way.What Personal Protective Equipment (PPE) Is Required
Forget the old days of wearing regular gloves and a lab coat. The current standard is strict:- Double chemotherapy-tested gloves-not just any nitrile. They must be tested and certified to resist permeation by antineoplastic agents. Change them every 30 minutes or immediately if torn.
- Impermeable gowns-not cotton. They must block liquid and vapor penetration. Disposable gowns are standard. Reusable ones require special laundering protocols.
- Eye protection-goggles or face shields if splashing is possible during mixing or administration.
- Respiratory protection-N95 masks or higher if aerosols are likely, such as during spill cleanup or when handling drugs like busulfan.
The Four-Step Verification Process: Your Last Line of Defense
The biggest change in the 2024 guidelines is the mandatory fourth verification step. Before, you had two people check the drug, the dose, and the patient. Now, you need a fourth check-done right at the bedside, in front of the patient. Here’s how it works:- Pharmacist verifies the order, dose, and compatibility.
- Nurse checks the drug against the prescription and patient’s chart.
- A second licensed clinician (RN, NP, or MD) confirms everything again.
- Fourth verification: At the bedside, two licensed clinicians use two patient identifiers (name and date of birth) to confirm identity, drug, dose, route, and time-out loud, in front of the patient.

Managing Cytokine Release Syndrome (CRS)
Immunotherapies like CAR-T and bispecific antibodies can trigger a dangerous immune overreaction called cytokine release syndrome. Symptoms: high fever, low blood pressure, trouble breathing. Left untreated, it kills 12-15% of patients. The 2024 standards now require every facility to have a CRS response plan ready. That means:- Monitoring vital signs every 15 minutes for the first hour after infusion.
- Having tocilizumab (Actemra) and corticosteroids immediately available.
- Training staff to recognize early signs-like a spike in temperature or drop in oxygen saturation.
- Documenting every intervention, even if the patient doesn’t progress to full CRS.
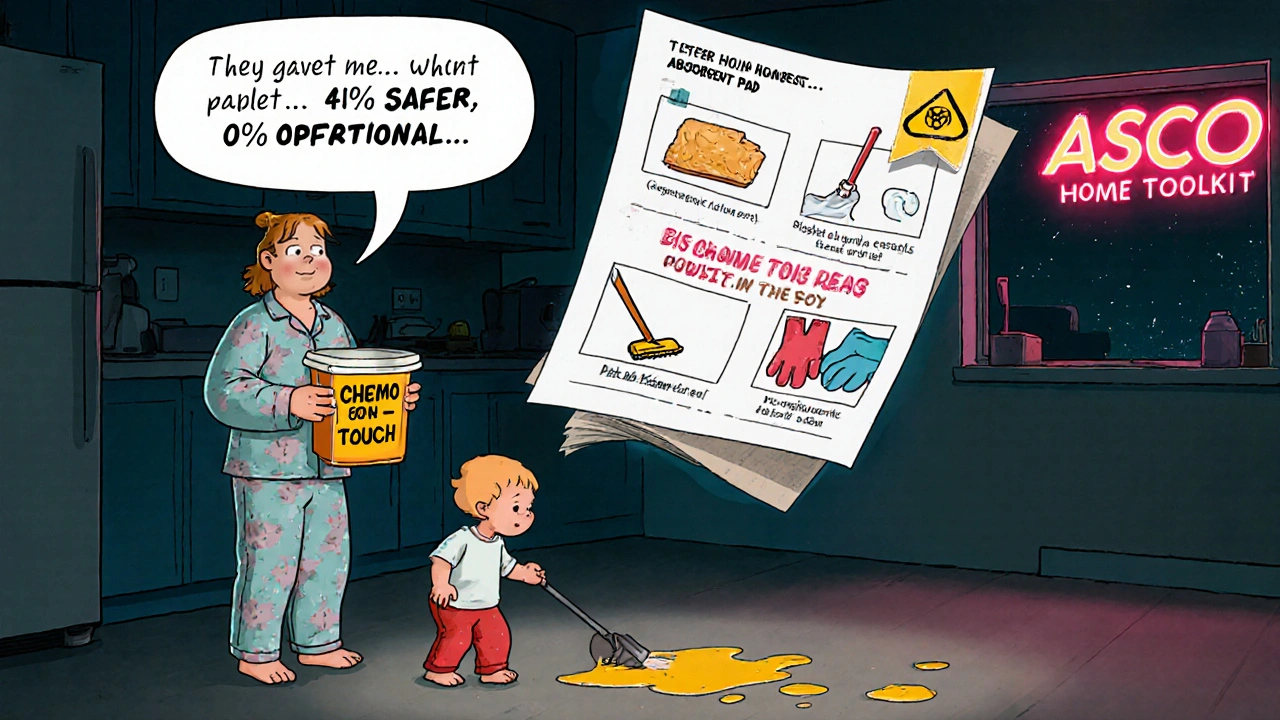
Home Chemotherapy: A Dangerous Gap
About 22% of home chemotherapy incidents involve improper waste disposal. Another 17% involve failed spill cleanup. Patients and caregivers are being sent home with drugs that can poison them if handled wrong-and too often, they’re given a pamphlet and told to “be careful.” The ASCO Chemotherapy Safety at Home toolkit helps. It includes:- Color-coded containers for bodily fluids (urine, vomit, stool) for 48-72 hours after treatment.
- Step-by-step spill kits with absorbent pads, gloves, and disposal bags.
- Clear instructions on how to wash laundry separately and flush toilets twice.
Costs and Barriers to Full Compliance
Implementing these standards isn’t cheap. A medium-sized oncology clinic needs:- $22,000-$35,000 for facility upgrades (ventilation, dedicated mixing rooms).
- $8,500-$12,000 for staff training and certification.
- $4,200-$6,800 per year for PPE and hazardous waste disposal.
- $15,000-$40,000 to modify EHR systems to support the four-step verification.
What Happens When You Skip the Rules
It’s not just about fines. It’s about lives. - A nurse who didn’t double glove developed ovarian cancer at age 38. She’d handled chemo for 12 years. Her case was documented by NIOSH. - A pharmacist reused gloves after mixing a drug. She contaminated a vial. Two patients got the wrong dose. One had a seizure. - A caregiver didn’t know how to clean a spill. Her toddler touched the floor after her mom vomited. The child tested positive for cyclophosphamide. These aren’t rare. They’re preventable. And they’re happening right now.How to Get Compliant
If your facility isn’t fully compliant, here’s how to start:- Assign a chemotherapy safety officer-someone with authority to enforce rules.
- Train every staff member: 8-12 hours initial, 4 hours annually. Pass a written test (85% minimum) and a hands-on skills check.
- Upgrade PPE and buy certified double gloves, impermeable gowns, and spill kits.
- Install CSTDs if possible. If not, document why and create a risk mitigation plan.
- Update your EHR to require the fourth verification step before dispensing.
- Create a CRS response protocol and run quarterly drills.
- Use the ASCO Home Safety Toolkit for every home care patient.
What’s Next?
By January 2025, the NCCN will require proof of fourth verification and CRS protocols for facility accreditation. By 2026, a national certification for chemotherapy handlers may become mandatory. AI-powered verification systems are already being piloted at 12 top cancer centers-tools that scan barcodes, confirm patient IDs, and auto-log steps to reduce human error. The future of chemotherapy safety isn’t just about better gear. It’s about smarter systems, better training, and equity. No patient should get safer care just because they live in a city. No nurse should risk their health because their clinic can’t afford a CSTD. The rules are clear. The tools exist. The data proves it works. The only thing left is to follow them.Do I need to double glove for all chemotherapy drugs?
No, but you need to know which ones require it. Drugs like carmustine, thiotepa, and busulfan are high-risk and require double chemotherapy-tested gloves. For others, single gloves may be sufficient if they meet NIOSH permeation standards. Always check the drug’s safety data sheet and your facility’s protocol. When in doubt, double glove.
Can I reuse chemotherapy gloves if they look clean?
Never. Even if gloves appear intact and clean, they can still contain microscopic traces of drugs that penetrate the material. Studies show contamination transfers within minutes. Always change gloves every 30 minutes during handling, and immediately if torn, punctured, or contaminated. Reusing gloves is a violation of USP <800> and ASCO/ONS 2024 standards.
What should I do if a chemotherapy spill occurs?
Follow your facility’s spill kit protocol. Put on double gloves, impermeable gown, eye protection, and respirator if aerosols are possible. Use absorbent pads to contain the spill. Never use paper towels. Place all contaminated materials in a hazardous waste bag labeled for antineoplastic agents. Decontaminate surfaces with detergent and water, then rinse. Document the spill, the cleanup, and any exposure. Report it to your safety officer immediately.
Is the fourth verification step really necessary if we’ve never made a mistake?
Mistakes aren’t always obvious. Many chemotherapy errors are caught before they cause harm-those are called near-misses. The fourth verification step catches misidentifications that slip through double-checks. In one facility, a nurse almost gave a drug to the wrong patient because both had similar names. The fourth check caught it. That’s why it’s mandatory. It’s not about past mistakes. It’s about preventing the next one.
How do I train caregivers for home chemotherapy safely?
Don’t just hand them a pamphlet. Demonstrate every step: how to handle vials, clean spills, dispose of syringes, and manage bodily fluids. Have them perform each task under supervision. Use the ASCO Chemotherapy Safety at Home toolkit. Confirm they can explain the process in their own words. Provide a 24/7 contact number for emergencies. Follow up within 48 hours. If they seem unsure, don’t send them home until they’re ready.
Are there alternatives to closed-system transfer devices (CSTDs) if my clinic can’t afford them?
CSTDs are the gold standard, but if cost is a barrier, you must implement other controls: use double gloving, work in a ventilated hood, minimize aerosol generation, and use pre-filled syringes when possible. Document your risk assessment and safety plan. But know this: without CSTDs, your exposure risk remains higher. The ASCO/ONS guidelines don’t excuse non-compliance due to cost-only mitigation. You must still reduce risk as much as possible.

