Choosing between basal-bolus and premixed insulin isn’t just about numbers on a glucose meter. It’s about whether you can stick with it when your schedule gets messy, when you’re tired, when your meals are late, or when your hands ache from arthritis. The right insulin regimen can mean the difference between feeling in control and feeling trapped.
How Basal-Bolus Insulin Works
Basal-bolus therapy is like having two separate insulin systems working together. One is a slow, steady background dose - the basal - that keeps your blood sugar stable between meals and overnight. The other is the bolus, a fast-acting shot you take before each meal to handle the sugar spike from food. Most people on this plan take four to five injections a day: one or two for basal, and one for each major meal.This setup gives you real flexibility. Need to skip breakfast? Skip the bolus. Eating a big pizza on Friday night? You can adjust your bolus dose based on carbs. It’s not magic - you need to count carbs, check your blood sugar before meals, and sometimes correct high readings with extra insulin. But if you’re someone who eats at different times every day, works night shifts, or likes to travel, this is the regimen that lets you live your life instead of rearranging it around your insulin.
How Premixed Insulin Works
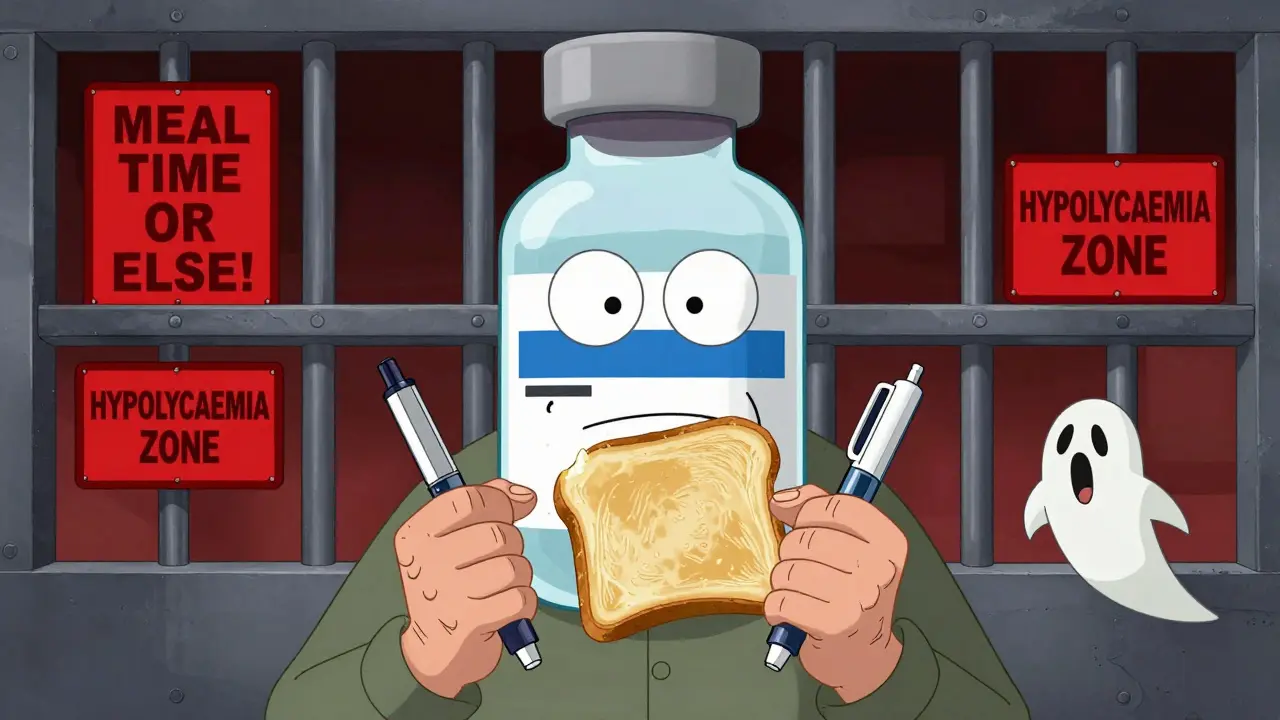
Premixed insulin is a pre-made blend - usually 70% longer-acting insulin and 30% faster-acting insulin - packaged in one syringe or pen. You get both background and mealtime coverage in a single shot. Most people take it twice a day: once before breakfast and once before dinner. That’s it. No extra doses. No carb counting. Just two injections, at two fixed times.That simplicity is why so many people - especially older adults or those with limited dexterity - start here. If you have arthritis, tremors, or trouble reading small labels, fewer injections mean less stress. But there’s a catch: you have to eat the same amount of carbs, at the same time, every day. Miss your lunch? You risk a low blood sugar. Eat a bigger dinner than usual? You might spike. There’s no room for spontaneity. If your life isn’t predictable, premixed insulin can feel like a cage.
Side Effects: Hypoglycemia Is the Real Issue
Both types can cause low blood sugar, but the risk isn’t the same. Studies show that people on premixed insulin have a higher chance of hypoglycemia - especially in the hours after meals or overnight. Why? Because the insulin peaks at fixed times. If you eat less than planned, or delay a meal, the insulin is still working hard and your blood sugar crashes.A 2015 hospital study had to be stopped early because over half the patients on premixed human insulin had low blood sugar episodes. Basal-bolus users had far fewer. That’s not because basal-bolus is safer by design - it’s because you can adjust. If your blood sugar is already low before a meal, you can skip the bolus. With premixed, you’re stuck with whatever dose you got.
But here’s the twist: if you use a continuous glucose monitor (CGM), the gap closes. People on premixed insulin with CGM have hypoglycemia rates almost as low as those on basal-bolus. The tech doesn’t fix the regimen - it just gives you early warnings so you can act.
Weight Gain: It’s Not as Big a Deal as You Think
Weight gain is a common fear with insulin. Both regimens can cause it, but basal-bolus tends to lead to slightly more - about 1.9 kg on average versus 1.0 kg with premixed. Why? Because basal-bolus users often take more total insulin to get tighter control. More insulin means your body stores more fat.But that’s not the full story. People on basal-bolus are also more likely to lose weight over time - not because of the insulin, but because they’re more aware of their food choices. They count carbs. They check numbers. They adjust. That awareness often leads to better eating habits. Premixed users, on the other hand, may eat the same meals every day without realizing how much sugar they’re consuming. The insulin masks the problem.
Lifestyle Fit: Flexibility vs Routine
This is where the real battle happens. Basal-bolus gives you freedom. You can sleep in. You can eat out. You can change your plans. But it demands more work. You need to learn carb counting. You need to check your blood sugar before every meal. You need to carry extra pens, test strips, and a logbook or app. It’s not just about injections - it’s about mental load.Premixed insulin demands less thinking. Two shots. Two meals. Stick to the plan. But if your life doesn’t follow a script - if you work irregular hours, care for kids, or travel often - this system breaks. One Reddit user wrote: “I switched from premixed to basal-bolus because I couldn’t handle the rigid meal schedule - missing a meal meant risking hypoglycemia even if my blood sugar was normal.”
Conversely, an older patient on the ADA forum said: “Two shots a day instead of four has made managing my diabetes possible since my arthritis makes multiple injections painful.”
Neither is right or wrong. It’s about matching the regimen to your life - not forcing your life to fit the regimen.
Who Should Choose What?
If you have type 1 diabetes, basal-bolus is almost always the standard. Your body doesn’t make insulin at all. You need precise control. If you have type 2 diabetes and your blood sugar spikes badly after meals, basal-bolus gives you the tools to fix it.Premixed insulin works best for people who:
- Have very regular meal times
- Don’t want to count carbs or check blood sugar before every meal
- Have trouble with fine motor skills or multiple daily injections
- Are older and prefer simplicity over precision
Doctors often push premixed because it’s easier to teach. A 2019 survey found only 42% of primary care doctors felt confident starting basal-bolus therapy. But that’s changing. With better insulin pens, smartphone apps, and CGMs, more people are moving to basal-bolus - even if they’re older.

Cost and Access
Premixed insulin is cheaper. On average, monthly out-of-pocket costs are $45.75 compared to $68.20 for basal-bolus, because you’re buying one product instead of two or three. In countries like India or parts of Southeast Asia, where insulin access is limited, premixed is the default. In the U.S. and Europe, basal-bolus use has grown 18% a year since 2018.Insurance matters. Some plans cover only premixed unless you prove you need more control. Others require you to try premixed first. Don’t assume your doctor knows your out-of-pocket costs. Ask. If cost is a barrier, talk to your pharmacist about patient assistance programs. Many insulin manufacturers offer free or low-cost options.
The Future: Hybrid and Smart Options
New options are emerging. In 2023, the FDA approved a “basal-plus” insulin - a single long-acting shot with the option to add a fast-acting dose only when needed. It’s not full basal-bolus, but it’s more flexible than premixed.Technology is lowering the barrier. Systems like Diabeloop use AI to suggest insulin doses based on your glucose trends, food intake, and activity. Early trials show patients using it need 27% fewer decisions per day. That’s huge. What used to take 10 minutes of math and guesswork now takes one tap.
By 2030, experts predict basal-bolus will be the standard in high-income countries - not because it’s perfect, but because it’s the most effective. And with smarter tools, it’s becoming easier to use.
What to Do Next
If you’re on premixed insulin and feel restricted - if you’re constantly worried about low blood sugar after skipping meals, or if you want to eat more freely - talk to your doctor about switching. You don’t have to stay stuck.If you’re on basal-bolus and overwhelmed - if counting carbs feels like a full-time job - ask about CGM. It reduces stress and hypoglycemia risk. Ask about insulin pumps or AI dosing tools. You’re not failing. The system just needs adjusting.
There’s no one-size-fits-all insulin. The best regimen is the one you can live with - without fear, without constant stress, without sacrificing your life.
Can I switch from premixed to basal-bolus insulin?
Yes, you can switch - and many people do. The transition usually takes a few weeks and requires close monitoring. Your doctor will start by replacing one of your premixed doses with a basal insulin shot, then gradually add bolus doses before meals. You’ll need to learn carb counting and blood sugar logging. Most people report better control and fewer lows after switching, especially if their meals are irregular.
Does basal-bolus insulin cause more weight gain than premixed?
Basal-bolus often leads to slightly more weight gain - about 1.9 kg on average versus 1.0 kg with premixed - because it allows tighter blood sugar control, which means your body stores more glucose as fat. But this isn’t inevitable. Many people on basal-bolus lose weight over time because they become more aware of their food choices. Weight gain isn’t caused by insulin alone - it’s caused by excess calories. Basal-bolus users often eat better because they track what they eat.
Is premixed insulin safer for elderly patients?
It can be - but only if their lifestyle is predictable. For seniors with arthritis, memory issues, or difficulty handling multiple injections, two daily shots are easier than four or five. But if they skip meals or eat inconsistently, premixed insulin raises the risk of dangerous low blood sugar. Many older adults do better with basal-bolus when supported by CGMs and simplified dosing tools. Safety isn’t about age - it’s about fit.
Can I use a CGM with premixed insulin?
Absolutely. In fact, using a CGM with premixed insulin significantly lowers your risk of low blood sugar. Studies show users with CGMs on premixed regimens have hypoglycemia rates nearly as low as those on basal-bolus. The CGM doesn’t change the insulin - it gives you early alerts so you can eat a snack or adjust your next dose. If you’re on premixed and having lows, a CGM is one of the best upgrades you can make.
Why do some doctors prefer prescribing premixed insulin?
Because it’s simpler to teach and easier to manage in busy clinics. Only 42% of primary care doctors feel confident starting basal-bolus therapy, compared to 78% for premixed. Premixed requires less patient education - no carb counting, no frequent testing. But that doesn’t mean it’s better. It just means it’s easier for doctors to prescribe. Ask if you’re a candidate for basal-bolus - especially if you’re struggling with rigid meal schedules or frequent lows.
Are there cheaper alternatives to basal-bolus insulin?
Yes. Some people use a basal-plus approach - one long-acting insulin shot daily, plus a fast-acting dose only when needed for meals. This reduces the number of daily injections and lowers cost compared to full basal-bolus. Generic insulins like NPH and regular insulin are also much cheaper than analogs. Talk to your pharmacist about biosimilars or patient assistance programs. Cost shouldn’t be a barrier to better control.



basal-bolus sounds like a full time job honestly i just want to eat and not do math before every bite
Of course the people who can afford CGMs and insulin pens with Bluetooth connectivity are the same ones who treat diabetes like a productivity hack. Meanwhile, my grandmother takes two shots a day and still manages to bake cookies for the church potluck. You call that a cage? I call it dignity.
Let’s not pretend that ‘flexibility’ is a universal good. Some of us don’t want to micro-manage every glucose spike. We want to live without being reminded we’re a broken machine every 90 minutes.
And yes, weight gain is real - but so is the psychological toll of being told your body’s natural rhythms are ‘irregular’ and therefore ‘suboptimal.’
It’s not about which regimen is better. It’s about who gets to decide what ‘better’ means.
Doctors push premixed because it’s easier. But we’re the ones who live with the consequences. Don’t mistake convenience for compassion.
It’s fascinating how the discourse around insulin regimens mirrors the broader neoliberal obsession with individual optimization. Basal-bolus isn’t just medical - it’s a performance of self-discipline. You’re not just managing glucose; you’re curating your metabolic identity.
The myth of ‘flexibility’ is a capitalist fantasy. You’re not free because you can skip breakfast - you’re free because you can afford the time, energy, and technology to optimize your biology. Most people don’t have that luxury.
Premixed insulin isn’t a failure of will. It’s a rational adaptation to a world that doesn’t accommodate biological unpredictability. The real villain isn’t the regimen - it’s the expectation that everyone must perform metabolic perfection.
And yes, CGMs help. But they also turn your body into a live dashboard. Is that liberation or surveillance?
Let’s stop glorifying the regimen that requires the most labor. The most ethical choice isn’t the most precise - it’s the one that respects human limits.
you guys are overthinking this so much
premixed works if you eat regular meals
basal bolus works if you wanna be a human glucose calculator
pick what dont make you wanna scream into a pillow every day
end of story
Anyone else notice how every single ‘expert’ here ignores the fact that insulin pricing is a cartel? Basal-bolus isn’t ‘better’ - it’s what Big Pharma wants you to buy. Premixed is cheaper because it’s older. They don’t want you to know that generic NPH + regular insulin can do 90% of what analogs do for 1/5 the cost.
And don’t get me started on CGMs. They’re great, sure - but only if your insurance covers them. Most people on Medicare or Medicaid get stuck with premixed because the system doesn’t care if you’re ‘trapped.’
This isn’t about lifestyle fit. It’s about who gets to be healthy. The rich get precision. The rest get survival.
Doctors push premixed? Of course they do - they’re paid per visit, not per outcome. They don’t want you coming back every week with questions. They want you quiet, compliant, and on the cheapest thing they can prescribe.
And now they’re selling ‘hybrid’ insulin like it’s innovation. It’s just repackaged control. The real breakthrough would be making insulin affordable for everyone - not giving the wealthy better tools to torture themselves with.
Thank you for this comprehensive and empathetic overview. It is imperative that we recognize diabetes management as a deeply personal and context-dependent endeavor, rather than a one-size-fits-all clinical protocol.
For individuals with limited dexterity, cognitive load, or socioeconomic resources, the simplicity of premixed insulin is not a compromise - it is a vital lifeline. The assumption that greater complexity equates to superior outcomes is not only medically unsound, but ethically problematic.
Conversely, for those with the capacity, support, and access to technology, basal-bolus therapy offers unparalleled precision and autonomy. This distinction must be honored, not pathologized.
Moreover, the integration of continuous glucose monitoring with any regimen significantly mitigates hypoglycemic risk, regardless of insulin type. Technology, when equitably distributed, serves as a great equalizer.
Healthcare providers must move beyond convenience-driven prescribing and engage in shared decision-making that centers patient values, daily realities, and cultural context.
Let us cease framing insulin regimens as moral choices. The best regimen is not the one that maximizes control - it is the one that preserves peace of mind.
Bro I'm from India and we don't even have access to basal-bolus unless you're rich. Premixed insulin is all we got and we still live. People here die because they can't afford insulin at all - not because they're not ‘flexible’ enough.
Stop acting like this is a lifestyle choice. This is a human rights issue. You talk about ‘trapped’? Try being trapped without medicine.
And don't even get me started on how Americans think their problems are universal. We don't have apps. We don't have CGMs. We have one vial of insulin that has to last two weeks. And we still wake up and take it.
So yeah, premixed might not be perfect. But it's the only thing keeping millions alive. Stop glorifying your fancy regimens while people here are rationing doses.
wait so if you use a cgm with premixed you get the same lows as basal bolus? so why even bother with 4 shots? just get the cgm and stick with 2
is this a scam? why is basal bolus even a thing if the tech makes premixed just as safe?
someone explain this to me