Over 19% of adults in the U.S. live with an anxiety disorder. That’s more than 1 in 5 people. Yet many still think it’s just "being nervous" or "overthinking." It’s not. Anxiety disorders are real, measurable, and treatable - but only if you know what you’re dealing with. This isn’t about feeling stressed before a presentation. This is about panic attacks that leave you gasping on the floor. About avoiding family dinners because your heart races at the thought of speaking. About spending hours checking the lock on your door, even though you know it’s closed. If you’ve ever felt trapped by your own mind, this is for you.
What Are the Main Types of Anxiety Disorders?
Anxiety isn’t one thing. It shows up in different forms, each with its own pattern. The DSM-5, the standard guide used by clinicians, recognizes seven major types. Some are well-known. Others are misunderstood - or overlooked entirely.Generalized Anxiety Disorder (GAD) is the most common. People with GAD don’t just worry - they worry constantly, about everything. Work. Health. Finances. Whether their kid made it to school safely. The worry isn’t tied to one event. It’s always there, like a low hum in the background. To be diagnosed, this has to last at least six months, and it has to interfere with daily life. About 3.1% of U.S. adults have it. Women are more likely to be affected.
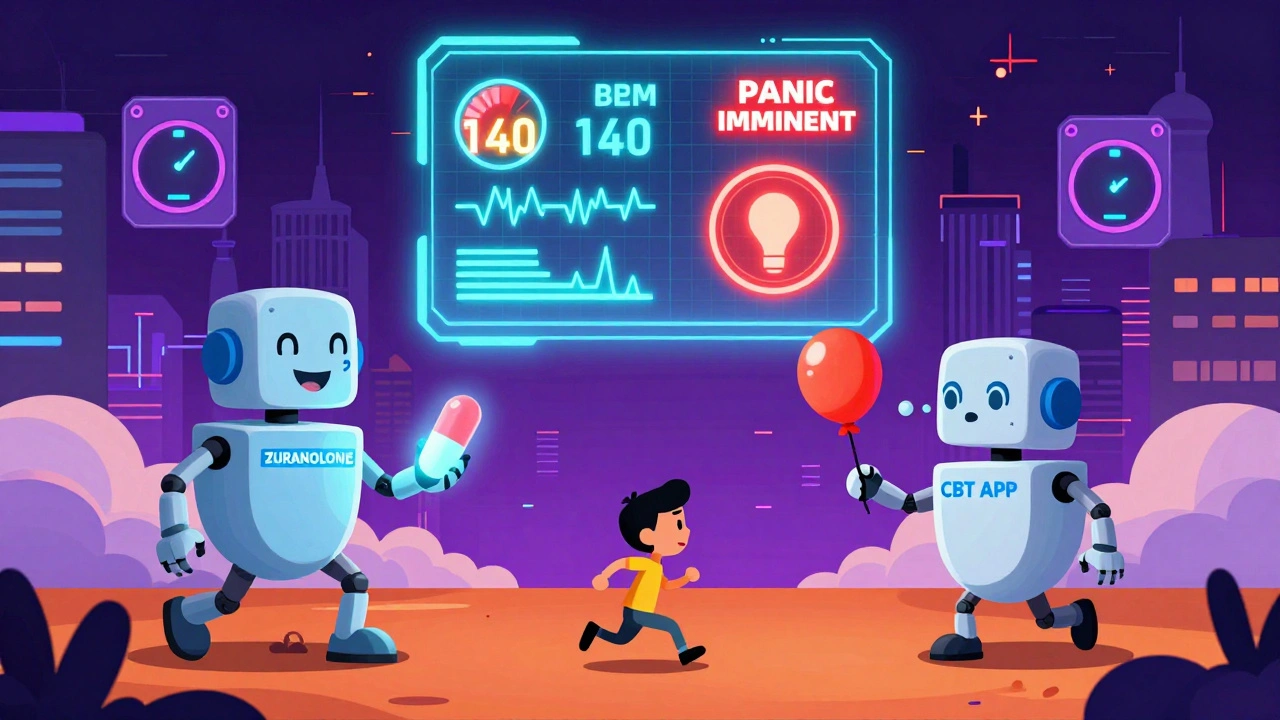
Panic Disorder is sudden, intense, and terrifying. You don’t need a trigger. One moment you’re fine. The next, your chest tightens, your heart pounds at 140 beats per minute, your hands shake, and you feel like you’re dying. These are panic attacks - and they’re not just "bad anxiety." They’re physical emergencies your brain falsely believes are real. About 2.7% of adults experience them. Many spend years thinking they have heart problems before getting the right diagnosis.
Social Anxiety Disorder isn’t shyness. It’s the fear that everyone is watching you, judging you, waiting for you to mess up. You avoid parties. You skip work meetings. You eat alone in your car because the cafeteria feels like a courtroom. This isn’t about being introverted. It’s about a paralyzing fear of humiliation. Around 7.1% of U.S. adults live with this - and many never tell anyone.
Specific Phobias are intense fears of specific things: spiders, heights, flying, needles, vomiting. The fear is out of proportion to the actual danger. You might know rationally that planes are safe. But your body doesn’t listen. 8.7% of adults have at least one specific phobia. Many live with them quietly, avoiding triggers instead of seeking help.
Obsessive-Compulsive Disorder (OCD) is now classified separately, but it still belongs here in practice. It’s not about being neat. It’s about intrusive thoughts - images, urges, doubts - that cause extreme distress. To calm the anxiety, you perform rituals: checking, washing, counting, repeating phrases. These aren’t habits. They’re desperate attempts to stop a mental storm. 1.2% of adults have OCD. Many hide it out of shame.
Separation Anxiety Disorder used to be seen as a childhood issue. Now we know adults get it too. You can’t sleep if your partner is out of town. You call your child every 15 minutes at school. You panic when your parent travels. The fear isn’t about being alone - it’s about losing someone you’re attached to. 4.1% of U.S. adults experience this.
Selective Mutism mostly affects children. They speak freely at home - but freeze completely at school or in public. It’s not defiance. It’s extreme anxiety that shuts down speech. Prevalence is low - under 2% - but it’s often misdiagnosed as autism or stubbornness.
What Do the Symptoms Really Look Like?
Symptoms aren’t just "feeling anxious." They’re physical, mental, and emotional - and they’re measurable.Physically, anxiety hits your body hard. During a panic attack, 92% of people report sweating. 87% tremble. 83% struggle to breathe. 76% feel dizzy. 68% get nauseous. Your heart rate spikes to 110-140 bpm - the same as during intense exercise. Your muscles tense. Your stomach knots. You might feel like you’re having a heart attack. That’s not coincidence. Your nervous system is stuck in fight-or-flight mode.
Cognitively, your brain goes into overdrive. 89% of people with GAD say they can’t concentrate. 82% have racing thoughts - a mental hamster wheel that won’t stop. 76% fall into catastrophic thinking: "If I make a mistake, I’ll lose my job, my partner will leave, I’ll end up homeless." 91% ruminate - replaying conversations, mistakes, or fears over and over. These aren’t choices. They’re automatic brain patterns shaped by fear.
Emotionally, you feel out of control. 95% of panic attack sufferers describe a sense of impending doom. 100% of GAD cases involve worry that’s disproportionate to reality. 88% fear they’ll lose control - scream, cry, pass out, or embarrass themselves in public. You might feel like you’re going crazy. You’re not. Your brain is just stuck in survival mode.
These symptoms don’t happen in isolation. They feed each other. A racing heart makes you think you’re having a heart attack. That thought increases anxiety. That increases heart rate. It’s a loop - and it’s exhausting.

What Treatments Actually Work?
The good news? Anxiety disorders respond well to treatment. Not always quickly. Not always easily. But they respond.Cognitive Behavioral Therapy (CBT) is the gold standard. It’s not talk therapy. It’s structured, skills-based training. You learn to identify distorted thoughts. You challenge them with evidence. You face fears gradually - not all at once. This is called exposure. For social anxiety, you might start by saying hello to a cashier. Then asking a question in a small group. Then giving a short presentation. For panic disorder, you might learn to breathe slowly while letting your heart race - to prove you won’t die. Studies show 50-60% of people see major improvement after 12-20 sessions. That’s better than medication alone.
SSRIs - like sertraline (Zoloft) and fluoxetine (Prozac) - are the first-line medications. They don’t work overnight. It takes 6-12 weeks. But when they do, they reduce physical symptoms, quiet racing thoughts, and improve sleep. Response rates are 40-60%. They’re safer than older drugs and don’t cause dependence. Side effects? Nausea, insomnia, or emotional numbness - especially early on. Many people quit too soon because they don’t give it time.
SNRIs like venlafaxine (Effexor) work similarly. They’re often used if SSRIs don’t help. They can be more effective for people with both anxiety and chronic pain.
Benzodiazepines - like Xanax or Klonopin - give fast relief. But they’re not a long-term solution. After a few months, your body builds tolerance. You need more to get the same effect. Withdrawal can be dangerous. Dependence happens in 15-30% of long-term users. They’re best for short-term crises - not daily management.
Acceptance and Commitment Therapy (ACT) is gaining ground. Instead of fighting thoughts, you learn to notice them without getting hooked. You focus on values - what matters to you - and take action anyway. It’s not about feeling better. It’s about living better, even with anxiety. Studies show it’s as effective as CBT.
What About Digital Tools and New Treatments?
Technology is changing how people manage anxiety.FDA-cleared apps like nOCD and Wysa guide users through CBT exercises. In 8 weeks, users report 35-45% symptom reduction - with just 20-30 minutes a day. These aren’t gimmicks. They’re structured programs backed by clinical data.
In 2023, the FDA approved zuranolone (Zurzuvae), the first oral drug specifically for postpartum anxiety. It works in days, not weeks. Early trials showed a 54% remission rate.
Research is also exploring ketamine-assisted therapy for treatment-resistant anxiety. In 2022 trials, 65% of patients saw rapid relief - within hours. It’s not widely available yet, but it’s a breakthrough.
AI tools are now predicting panic attacks 24 hours in advance with 87% accuracy - by analyzing breathing patterns, heart rate, and movement. This could lead to early interventions before a full attack hits.
And in 2023, researchers identified three distinct "anxiety biotypes" using brain scans. Each responds differently to treatment. This means future care could be personalized - not trial-and-error.
Why Do So Many People Still Struggle?
Even with proven treatments, many don’t get better.A 2022 VA survey of 12,500 patients found only 37% reached remission after six months. Why? Two big reasons: access and dropout.
Wait times for specialized therapists? 6-8 weeks. Insurance limits? Often 10 sessions a year. Many can’t afford out-of-pocket costs. Others start treatment, then quit because exposure therapy feels unbearable. One Reddit user wrote: "CBT helped, but exposure made me want to quit. I felt like I was breaking myself." That’s normal. It’s hard. But it’s also the part that works.
Medication side effects turn people off. Some feel emotionally flat. Others gain weight. One person switched from an SSRI to buspirone - a non-addictive anti-anxiety drug - and found relief without numbness.
The biggest barrier? Shame. Many think anxiety is weakness. They hide it. They suffer alone. But anxiety doesn’t care about your job title, your income, or how "strong" you think you are. It’s a biological condition - like diabetes or high blood pressure.
What Can You Do Right Now?
You don’t have to wait for therapy to start feeling better.Start with breathing. Diaphragmatic breathing - slow, deep breaths at 5-6 per minute - calms your nervous system in minutes. Try it now: inhale for 4 seconds, hold for 2, exhale for 6. Repeat 5 times.
Write down your thoughts. Not to fix them. Just to get them out. You’ll start seeing patterns. "I always think I’ll fail when I speak up." That’s not truth. That’s anxiety.
Move your body. Even a 15-minute walk reduces cortisol. Exercise is a natural SSRI.
Find support. NAMI’s 24/7 helpline answers 25,000 calls a month. The ADAA hosts 300+ weekly support groups. You’re not alone.
And if you’re ready - find a therapist who specializes in CBT or ACT. Don’t settle for general counselors. Ask: "Do you use exposure therapy for anxiety?" If they don’t know what you mean, keep looking.
Anxiety doesn’t have to rule your life. It can be managed. Treated. Reduced. Even silenced - not by willpower, but by science.
Can anxiety disorders go away on their own?
Rarely. While some people experience less intense symptoms over time, untreated anxiety disorders usually persist or worsen. The brain learns to stay in high-alert mode. Without intervention, avoidance behaviors strengthen the fear. Studies show that without treatment, over 70% of people with GAD or panic disorder still have significant symptoms five years later. Early treatment improves long-term outcomes dramatically.
Is medication necessary for treating anxiety?
Not always - but it helps many. For mild to moderate cases, CBT alone can be enough. For severe cases - especially with panic attacks, depression, or physical symptoms - medication often speeds up recovery. SSRIs don’t make you "happy." They reduce the noise so therapy can work. Many people use medication short-term, then taper off after building coping skills. Others stay on it long-term, like someone with high blood pressure. There’s no shame in either choice.
How long does CBT take to work?
Most people start noticing changes in 4-6 weeks. By session 12, 60-80% report significant improvement. But real change takes practice. You’re rewiring your brain. That doesn’t happen overnight. The first few weeks are often the hardest - exposure feels scary. But the more you do it, the less power fear has. Think of it like physical therapy: painful at first, but the results last.
Can children have anxiety disorders?
Yes - and often earlier than you think. Half of all anxiety disorders begin by age 11. Children may not say "I’m anxious." They might throw tantrums, refuse school, cling to parents, or complain of stomachaches. Selective mutism and separation anxiety are common in kids. CBT adapted for children - using play, stories, and rewards - is highly effective. Early treatment prevents lifelong struggles.
Why do some people get anxiety and others don’t?
It’s a mix of biology and experience. Genetics play a role - if a parent has anxiety, you’re 2-3 times more likely to develop it. Brain chemistry, especially serotonin and GABA levels, affects how you process fear. Trauma, chronic stress, or early life adversity can trigger it. But it’s not your fault. You didn’t choose this. You’re not broken. You’re just wired differently - and that wiring can be rewired.
What’s the difference between anxiety and stress?
Stress is a reaction to a specific situation - a deadline, a fight, a job interview. It goes away when the situation ends. Anxiety is persistent. It’s worry that lingers without a clear trigger. You feel anxious even when everything’s fine. Stress is about the future. Anxiety is about imagining worst-case scenarios - even when there’s no evidence. Stress can motivate. Anxiety paralyzes.


Okay but have you considered that anxiety is just the government’s way of keeping us docile? The CDC’s stats are fabricated to sell SSRIs. I know someone who ‘got better’ after she stopped eating gluten and started wearing a copper bracelet aligned with the moon’s phases. The real cure is energy healing - but Big Pharma doesn’t want you to know that. 🤫
What’s interesting is how we’ve medicalized human suffering. Anxiety isn’t a disorder - it’s a signal. A signal that our society is broken. We’re overworked, disconnected, and terrified of stillness. CBT helps, sure - but what if the real treatment is rebuilding community? Slowing down? Letting people just… be? The brain doesn’t need fixing. It needs belonging.
Oh my god. I just read this and I’m crying. Not because I’m dramatic - but because I’ve lived every single sentence. The panic attacks in the grocery store. The 3 a.m. spirals where I convinced myself my cat was judging me. The way I’d rehearse saying ‘hi’ to my neighbor for 20 minutes before actually doing it. I didn’t know it had a name. I thought I was broken. Thank you for writing this. I’m finally seeing it: I’m not weak. I’m just wired differently. And that’s okay.
...This article is 98% fluff. You cite DSM-5 like it’s scripture. You mention ‘evidence-based’ but ignore that 40% of CBT studies are funded by pharma. Also, ‘diaphragmatic breathing’? Really? That’s your solution? And you call benzodiazepines ‘dangerous’ - but never mention how many people overdose on opioids while on SSRIs? You’re not helping. You’re performing.
I’m from Nigeria, and here, anxiety is called ‘too much thinking’. People say, ‘Pray more’. But I’ve seen friends collapse from it. I didn’t know it was medical until I moved to the U.S. for school. This post helped me understand my sister - she never spoke in class, always sat alone. Now I know it was selective mutism. Thank you for naming it. I’m taking her to a therapist next week.
You misused ‘DSM-5’ as a proper noun. It’s ‘DSM-5’ - not ‘the DSM-5’. Also, you say ‘anxiety isn’t just being nervous’ - but then you use ‘nervous’ in the same paragraph as ‘panic attacks’. That’s not precise. And ‘low hum in the background’? Poetic. But unscientific. Also - ‘your brain is stuck in fight-or-flight mode’? That’s not a mechanism. It’s a metaphor. Fix your language before you fix the world.
Lol. This is why America’s falling apart. We’ve turned feelings into diagnoses. Next thing you know, being tired is ‘chronic fatigue syndrome’ and being sad is ‘major depressive disorder’. Just grow a spine. I’ve had anxiety my whole life. I didn’t need a 12-session CBT program. I needed to stop being a baby. Do push-ups. Get a job. Shut up.
omg i literally cried reading this. i thought i was just ‘weird’ for avoiding parties. now i know it’s social anxiety. also, the part about checking the door 10 times?? me. every. single. night. i’m finally gonna make that therapist appointment. thanks for not making me feel like a freak.
thank you for this ❤️ i was scared to tell anyone i feel like my mind is a broken record. now i know its OCD. im gonna try the nOCD app. i believe in you! 🙏
I’ve been on Zoloft for 8 months. It made me feel like a zombie. I cried every day for no reason. I stopped taking it. Then I started journaling, walking in the woods, and screaming into pillows. I didn’t need meds. I needed to feel my feelings. This article made me feel seen - but the ‘treatments’ listed? Most of them just numb you. I’m not broken. I’m just hurting.
USA best country for mental health care 🇺🇸😂 Look at all these people crying over breathing exercises. In Russia they just drink vodka and deal with it. In China they work 18 hours and forget they’re anxious. We’re soft. Fix yourself. No therapy needed. #MakeAnxietyGreatAgain