Antihistamine Guide for Eczema
Antihistamines block histamine, which causes itch. They're most helpful for:
- Allergic flares
- Nighttime itching
- Pruritic dermatitis in children
Note: They don't treat underlying inflammation.
Enter your situation to get personalized recommendations.
| Antihistamine | Sedation | Duration | Best For |
|---|---|---|---|
| Diphenhydramine | High | 4-6 hrs | Bedtime |
| Cetirizine | Low | 24 hrs | Daytime |
| Loratadine | Minimal | 24 hrs | General |
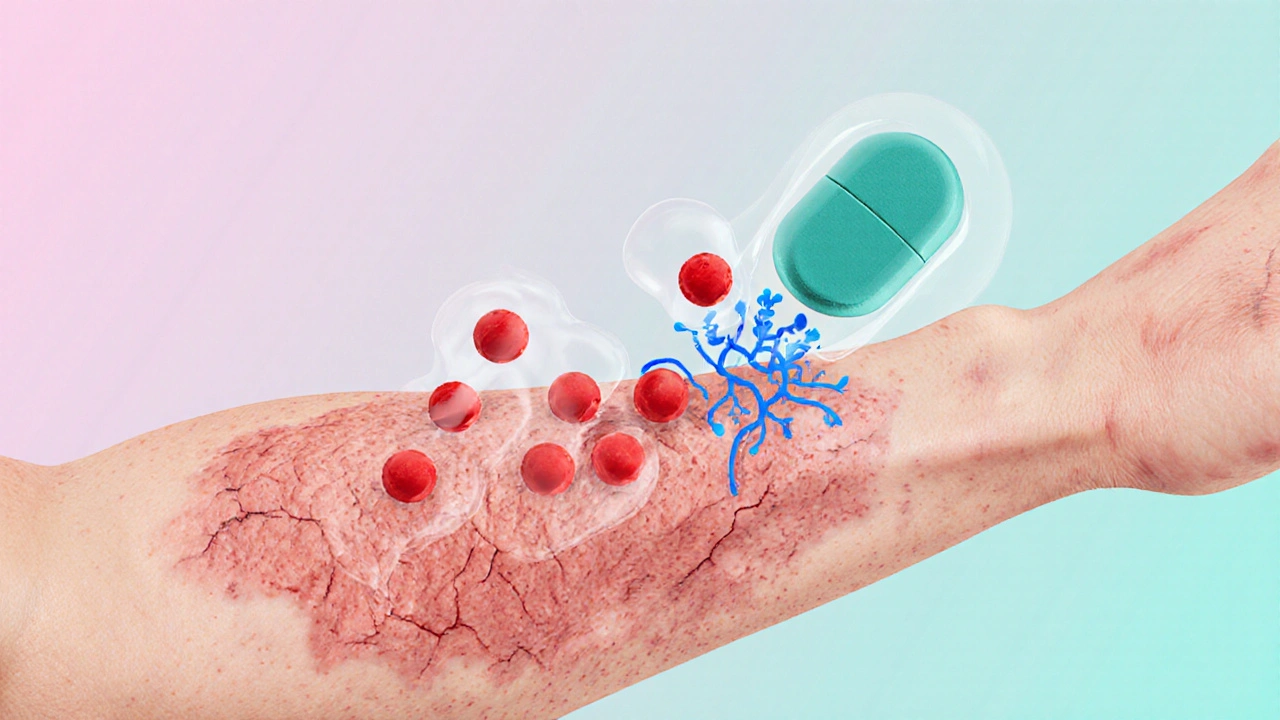
Living with eczema means battling relentless itch, flaky skin, and the frustration of flare‑ups that seem to appear out of nowhere. While moisturizers and steroids are front‑line tools, many patients wonder if a simple antihistamines for eczema can calm the itch and speed recovery. Below we unpack exactly how antihistamines fit into eczema management, when they’re truly useful, and what you should watch out for.
Antihistamines are drugs that block the action of histamine, a chemical released during allergic reactions. Histamine binds to receptors on nerve endings, sending itch signals to the brain. In eczema, the itch‑scratch cycle can be intensified by histamine spikes, especially during allergic flares. By dampening this signal, antihistamines can reduce the urge to scratch, giving the skin a better chance to heal.
Eczema (also called atopic dermatitis) is a chronic inflammatory skin condition characterized by dry, itchy patches and a tendency to flare with triggers like stress, allergens, and temperature changes. The condition involves a broken skin barrier, immune dysregulation, and heightened sensitivity to irritants. Because itch is the most debilitating symptom, any therapy that can break the itch‑scratch loop deserves a close look.
How Antihistamines Work in Eczema
Antihistamines fall into two major families based on the receptors they block:
- H1 receptor antagonists (commonly called "antihistamines") target the H1 histamine receptor on nerve fibers, directly reducing itch.
- H2 receptor antagonists affect stomach acid production but have modest anti‑inflammatory effects that can complement skin treatment.
When you take an H1 blocker, it competes with histamine for the receptor, essentially turning down the volume on the itch signal. This doesn’t fix the underlying inflammation, but it buys time for moisturizers, topical steroids, or immune‑modulating drugs to do their work without the skin being constantly broken by scratching.
When Antihistamines Are Actually Helpful
Not every eczema patient needs an antihistamine. Clinical experience and recent guidelines suggest they’re most beneficial in these scenarios:
- Allergy‑driven flares. If you notice worsening itch after exposure to pet dander, pollen, or dust mites, an oral antihistamine can curb the histamine surge.
- Nighttime itching. Sedating first‑generation antihistamines like diphenhydramine are often used at bedtime to help patients get an uninterrupted sleep.
- Pruritic dermatitis in children. Low‑dose cetirizine or loratadine is sometimes prescribed when topical steroids alone don’t control scratching.
For pure dry‑skin itch without an allergic trigger, antihistamines usually add little benefit and may expose you to unnecessary side effects.
First‑Generation vs. Second‑Generation Oral Antihistamines
Choosing the right pill often comes down to balancing effectiveness with side‑effects like drowsiness. Below is a quick comparison of the most common options.
| Attribute | First‑Generation (e.g., Diphenhydramine, Chlorpheniramine) | Second‑Generation (e.g., Cetirizine, Loratadine, Desloratadine) |
|---|---|---|
| Typical Sedation | High - common to feel sleepy | Low to none |
| Duration of Action | 4‑6hours | 24hours (once‑daily dosing) |
| OTC Availability (U.S.) | Yes | Yes |
| Common Dose for Adults | 25‑50mg every 6‑8h | 10mg once daily (Cetirizine) or 10mg daily (Loratadine) |
| Typical Side Effects | Dry mouth, drowsiness, dizziness | Headache, mild GI upset |
For nighttime itch, many clinicians still reach for a first‑generation agent because the drowsiness is a bonus. During the day, second‑generation drugs are preferred to keep you alert while still blunting the itch.

Dosing, Safety, and Common Side Effects
Even “over‑the‑counter” antihistamines can cause problems if used incorrectly. Here’s a quick cheat sheet:
- Start low. For adults, begin with the lowest recommended dose and see how your skin and alertness respond.
- Watch for sedation. If you feel drowsy, switch to a second‑generation agent or limit the dose to bedtime.
- Kid safety. Children under 6years generally need pediatric‑specific formulations; dosing is weight‑based (e.g., cetirizine 2.5mg for a 20‑lb child).
- Pregnancy & lactation. Consult your OB‑GYN; many providers favor loratadine as the least risky option.
- Drug interactions. Antihistamines can amplify the sedative effect of alcohol, benzodiazepines, and some antidepressants.
Rare but serious side effects-like heart rhythm changes with high‑dose first‑generations-should prompt immediate medical review.
Combining Antihistamines with Standard Eczema Therapies
Antihistamines are most powerful when layered on proven eczema treatments:
- Moisturizers. Maintaining a hydrated barrier reduces the frequency of itch triggers.
- Topical corticosteroids. Short courses (e.g., hydrocortisone 1% for mild flares, clobetasol for severe lesions) calm inflammation, while antihistamines keep the itch from undoing the work.
- Calcineurin inhibitors. Tacrolimus or pimecrolimus can be used on sensitive areas; antihistamines help patients tolerate the temporary burning sensation.
- Immune modulators. For moderate‑to‑severe eczema, biologics like dupilumab dramatically lower disease activity; antihistamines may still aid nighttime comfort during the induction phase.
Think of antihistamines as the “assistant” that lets the main treatments perform without interruption.
Special Populations: Kids, Seniors, and Pregnant People
Children often experience more intense itch, but their livers process drugs differently, so pediatric dosing is crucial. Low‑dose cetirizine (2.5mg) or levocetirizine is commonly chosen because it avoids the heavy sedation of diphenhydramine.
Older adults may already be on multiple medications that cause drowsiness. A non‑sedating second‑generation antihistamine is the safest bet, and starting with half the adult dose can prevent falls.
Pregnant patients should avoid first‑generation antihistamines unless absolutely necessary. Current guidelines point to loratadine as the preferred option because it has the most safety data in pregnancy.
Key Takeaways
- Antihistamines help mainly by reducing histamine‑driven itch; they don’t treat the underlying inflammation.
- Use them for allergy‑related flares, nighttime itching, or when topical therapies aren’t enough.
- Second‑generation agents (cetirizine, loratadine) are best for daytime use; first‑generation drugs are useful at bedtime but cause drowsiness.
- Always pair antihistamines with moisturizers, steroids, or biologics for a comprehensive approach.
- Watch dosing, especially in children, seniors, and pregnant individuals, and be aware of drug interactions.

Frequently Asked Questions
Can I use antihistamines every day for eczema?
Daily use is okay for many patients, especially with a non‑sedating second‑generation drug. However, you should reevaluate every few months with your dermatologist to ensure the medication is still needed and to monitor any side effects.
Do antihistamines work for non‑allergic eczema?
If histamine isn’t a major driver, antihistamines provide limited relief. In such cases, focusing on barrier repair and anti‑inflammatory treatments is more effective.
Is it safe to combine two antihistamines?
Generally, no. Stacking antihistamines increases the risk of sedation, dry mouth, and heart rhythm issues. Stick to a single agent and adjust the dose if needed.
What should I do if I feel drowsy after taking an antihistamine?
Switch to a non‑sedating second‑generation product or limit the medication to bedtime. If drowsiness persists, talk to your doctor about a dose reduction.
Are there natural alternatives to antihistamines for itch?
Cool compresses, colloidal oatmeal baths, and topical menthol can soothe itch, but they don’t block histamine. These methods work best as adjuncts to medical therapy.

Your guide glosses over the fact that most eczema patients don’t benefit from antihistamines at all.
Hey, I get where you’re coming from 🙌. Antihistamines can be a useful adjunct for those who have clear allergic triggers, but they’re definitely not a magic bullet. If you pair them with a solid moisturizer routine, the skin barrier improves and the itch drops off faster. 😊 Just remember to pick a non‑sedating option for daytime use so you stay alert at work.
Totally agree that you need a holistic approach – moisturizers, steroids, and maybe an antihistamine if the itch is histamine‑driven. 🌟 Keep tracking what triggers your flares; it’ll help you decide when the pill is actually needed.
Let’s dissect the premise that antihistamines are a cornerstone of eczema therapy. First, the pathophysiology of atopic dermatitis is driven predominantly by a Th2‑mediated immune response, not histamine release per se. Second, clinical trials repeatedly demonstrate that H1 blockers provide marginal benefit in non‑allergic eczema. Third, the sedative properties of first‑generation agents can impair daily functioning, especially in students and professionals. Fourth, reliance on antihistamines may delay escalation to proven anti‑inflammatory treatments. Fifth, pediatric dosing errors are common, leading to either sub‑therapeutic effects or unnecessary sedation. Sixth, in the elderly, anticholinergic burden adds to fall risk. Seventh, pharmacists often dispense these drugs over‑the‑counter without reinforcing the importance of barrier repair. Eighth, insurance formularies sometimes favor cheap antihistamines, creating a false sense of adequacy. Ninth, patients may misinterpret “no side‑effects” as “no risk.” Tenth, the placebo effect can mask lack of true efficacy. Eleventh, combining antihistamines with topical steroids does not synergize pharmacodynamically; it merely adds convenience. Twelfth, long‑term safety data for chronic antihistamine use in eczema is sparse. Thirteenth, regional guidelines such as those from the American Academy of Dermatology advise using antihistamines only for specific histamine‑mediated itch. Fourteenth, practitioner education must emphasize this nuance to prevent overprescription. Fifteenth, the bottom line is that antihistamines are a niche tool, not a universal solution.
Great points, Subramaniam. To add a practical tip, if you decide to try a second‑generation antihistamine, take it after a meal to minimize any stomach upset. Also, keep a simple diary noting itch intensity before and after dosing; this objective data can help your dermatologist tweak the regimen. 🌱
From a cultural perspective, it’s fascinating how different societies approach itch management. In many East Asian traditions, herbal teas containing chamomile or licorice root are used alongside topical oils, reflecting a holistic view of skin health. Meanwhile, in Mediterranean regions, patients often rely on olive oil moisturizers and a diet rich in omega‑3 fatty acids, believing that internal inflammation mirrors cutaneous symptoms. In contrast, Western medicine has favored a pharmacologic model, emphasizing topical steroids, calcineurin inhibitors, and, when indicated, antihistamines to quell the itch‑scratch cycle. This dichotomy underscores the importance of patient education: understanding that antihistamines target histamine pathways, which are only a fragment of the inflammatory cascade in eczema. Moreover, the psychosocial context cannot be ignored; stress‑induced flares are common, so integrating mindfulness or yoga can complement pharmacotherapy. Nutrition also plays a role; emerging evidence suggests that reducing dairy and gluten may benefit susceptible individuals, though the data remain inconclusive. Lastly, community support groups-whether online forums or local meet‑ups-provide shared experiences that help patients navigate the trial‑and‑error nature of treatment choices. In sum, while antihistamines have a place, they should be woven into a broader tapestry of lifestyle, cultural practices, and evidence‑based medicine for optimal skin health.
Whilst the article is exhaustive, its tone oscillates between clinical manual and marketing brochure, lacking the gravitas expected of a dermatological discourse. The excessive use of promotional phrasing ("assistant" to treatments) dilutes the scientific rigor. A more balanced narrative would juxtapose the modest efficacy of antihistamines with the robust data supporting barrier restoration therapies.
Indeed; balance is essential; however, the article does provide valuable data; readers benefit from concise tables; the inclusion of dosage specifics is laudable; yet, a clearer distinction between first‑ and second‑generation agents would improve usability.
Look, the guide totally misses the point that many patients just need proper moisturizers, not a pill that makes them nap all day. Stop pushing drugs and focus on skin care basics.
Hey there! Totally hear you on the moisturizer angle 😊. A solid regimen of gentle cleansers and fragrance‑free creams can cut down the need for any extra meds. Keep it simple and your skin will thank you!
Honestly, the whole antihistamine hype feels like a marketing ploy; the evidence is thin, and most people are better off with barrier repair alone.
Gotcha, Lindy! 🎉 Still, a tiny dose at night can be a game‑changer for those who can’t sleep because of itch. Just pick a low‑sedation option and you’re golden.
Antihistamines help only when histamine is the culprit; otherwise they’re wasted.
Consider the itch as a messenger, not an enemy; when we listen to what it tells us about internal imbalance, we can address the root rather than silencing the signal.
The article covers the basics well, but remember to personalize the regimen; what works for one might not work for another.
While some swear by antihistamines, many find they add unnecessary sedation; choose wisely.
Note: "antihistamine" is singular; "antihistamines" is plural. Consistency in terminology enhances readability.