For years, millions of people have reached for over-the-counter painkillers like ibuprofen, naproxen, or Excedrin without a second thought. They’re cheap, easy to find, and seem harmless. But if you’ve been taking them daily for years-especially in combination with caffeine or codeine-you could be silently damaging your kidneys. This isn’t theory. It’s analgesic nephropathy, a preventable form of chronic kidney disease caused by long-term overuse of common pain medications.
What Exactly Is Analgesic Nephropathy?
Analgesic nephropathy is kidney damage from taking too much pain medicine over a long time. It’s not sudden. It doesn’t hurt at first. You won’t feel it until your kidneys are already struggling. The damage builds up slowly, like rust on a pipe you never clean. By the time symptoms show up-fatigue, swelling, high blood pressure-it’s often too late to reverse.
This condition became well-known in the 1970s and 80s when people regularly took combination painkillers with phenacetin, a now-banned ingredient. But even after phenacetin disappeared from shelves, the problem didn’t go away. Today, it’s mostly caused by NSAIDs like ibuprofen and naproxen, and sometimes by too much acetaminophen. The real danger? People don’t realize they’re at risk because these drugs are sold without a prescription.
What happens inside your kidneys? NSAIDs block chemicals that help keep blood flowing to your kidneys. Less blood flow means less oxygen, more stress, and eventually, tissue death in the inner parts of the kidneys called papillae. Over time, this leads to scarring, reduced kidney function, and sometimes complete failure. The process is silent. You won’t feel it until your creatinine levels spike during a routine blood test.
Who’s Most at Risk?
You might think this only affects older adults or people with existing kidney problems. But the truth is, it’s most common in women between 35 and 55. Why? Many manage chronic headaches, menstrual pain, or arthritis with daily painkillers. A 2021 study found that 72% of diagnosed cases were women. And it’s not just about how much you take-it’s how often.
Here’s the red flag: if you’ve been taking six or more pain pills a day for three years or more, your risk jumps sharply. Even more concerning? Combination products. Excedrin, for example, contains acetaminophen, aspirin, and caffeine. Studies show these combinations are 3.7 times more likely to cause kidney damage than single-ingredient pills. Caffeine makes the problem worse by increasing blood pressure and reducing kidney blood flow even further.
People with high blood pressure, diabetes, or already reduced kidney function are at even higher risk. But here’s the scary part: 62% of patients diagnosed with analgesic nephropathy had no idea their painkillers could hurt their kidneys. They thought, “It’s just Tylenol.”
How Do Doctors Diagnose It?
There’s no single test. Diagnosis comes from piecing together your history, lab results, and imaging. If you’ve been taking NSAIDs daily for years and your blood tests show rising creatinine or low estimated glomerular filtration rate (eGFR), your doctor will suspect kidney damage.
Urinalysis often shows mild protein in the urine (less than 3.5 grams per day) and no signs of infection or blood-what doctors call “bland sediment.” That’s unusual. Most kidney problems show blood or white cells in the urine. This quiet pattern is a clue.
The most telling sign? Calcifications in the renal papillae. A noncontrast CT scan picks these up with 87% accuracy. These calcium deposits are the fingerprints of long-term analgesic abuse. They’re not always visible early on, which is why routine blood work is so important. If your doctor doesn’t check your kidney function every six months while you’re on long-term pain meds, ask why.
NSAIDs vs. Acetaminophen: Which Is Safer?
Many people believe acetaminophen (Tylenol) is the safe alternative to NSAIDs. It’s not. While it doesn’t reduce kidney blood flow like NSAIDs do, it still carries risk when used excessively.
A 2020 study in Kidney International Reports found that people who took more than 4,000 mg of acetaminophen daily for five or more years had a 68% higher chance of developing chronic kidney disease than non-users. That’s not a small risk. It’s the same as smoking a pack a day for 10 years.
NSAIDs like ibuprofen and naproxen are worse for blood flow. At normal doses, they cut kidney blood flow by 25-40%. At high doses, that jumps to 50-70%. Acetaminophen doesn’t do that. But it overwhelms the liver’s ability to detoxify, creating harmful byproducts that stress the kidneys. So neither is truly safe with long-term, daily use.
The real problem isn’t one drug. It’s the habit. Taking painkillers every day for years, whether it’s Advil, Tylenol, or Excedrin, is the pattern that breaks your kidneys.
What Happens If You Stop?
The good news? If caught early, the damage can stop-and sometimes even reverse.
A 2022 study followed 142 patients who stopped all NSAIDs and acetaminophen as soon as their kidney damage was diagnosed. After five years, 73% had stabilized kidney function. None got worse. That’s huge. Most chronic kidney diseases keep declining. But analgesic nephropathy? It can pause.
One Reddit user, ‘ChronicPainWarrior99,’ shared their story: “I took 8-10 Excedrin Migraine tablets a day for seven years. My GFR dropped to 45. My nephrologist said I was lucky it wasn’t worse.” He stopped. His numbers didn’t improve, but they didn’t get worse either. That’s the goal: stop the decline.
But here’s the catch: stopping painkillers doesn’t mean stopping pain. Many patients report a major drop in quality of life after quitting. One survey found that 41% struggled to find effective alternatives. That’s why switching to safer methods isn’t optional-it’s essential.
Safer Ways to Manage Chronic Pain
You don’t have to suffer. There are effective, kidney-safe options.
- Topical NSAIDs: Gel or patch versions of diclofenac or ibuprofen deliver pain relief directly to the joint or muscle. Systemic absorption drops by 90%. A 2021 trial showed they worked just as well as pills-with zero impact on kidney function.
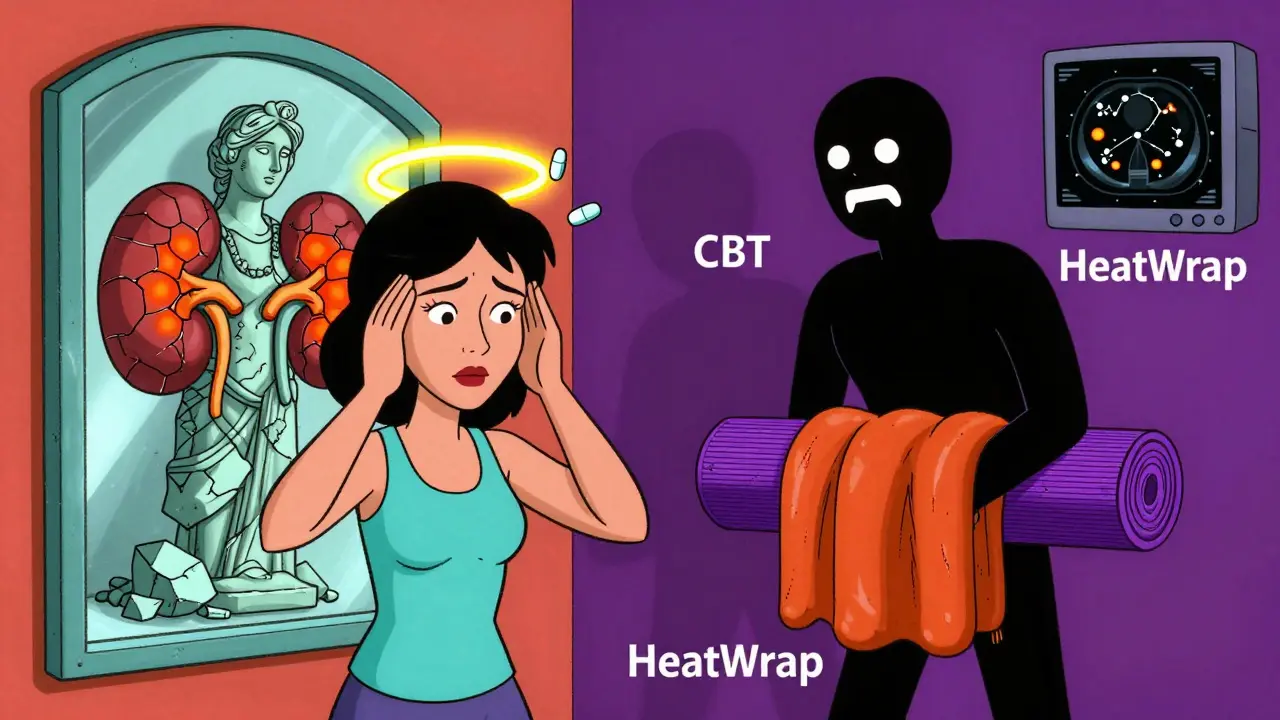
- Heat therapy: ThermaCare HeatWraps or heating pads reduce osteoarthritis pain by 40-60%. No chemicals. No risk. FDA-cleared and proven in clinical studies.
- Physical therapy: Strengthening muscles around painful joints reduces pressure and inflammation. The American College of Rheumatology recommends trying PT for 4-6 weeks before even considering pills.
- Cognitive behavioral therapy (CBT): Chronic pain changes your brain. CBT helps rewire how you respond to pain signals. Studies show it reduces pain intensity as effectively as opioids-with no side effects.
- Low-dose antidepressants: Duloxetine (Cymbalta) is FDA-approved for chronic musculoskeletal pain. It works on nerve pain pathways, not inflammation. Safe for kidneys.
For migraines, new prescription drugs called CGRP inhibitors (like Aimovig or Emgality) block the nerve signals that trigger attacks. They cost about $650 a month, but they don’t touch your kidneys. If you’re on daily painkillers for migraines, this is worth discussing with your doctor.

What You Should Do Today
Here’s your action plan:
- Count your pills. How many NSAIDs or acetaminophen do you take in a week? If it’s more than three days, you’re in the danger zone.
- Check your labels. Avoid combination products. If it says “Excedrin,” “Midol,” or “Anacin,” it contains caffeine or multiple painkillers. These are the worst offenders.
- Set limits. Never take more than 3,000 mg of acetaminophen a day. Never exceed 1,200 mg of ibuprofen or 750 mg of naproxen daily for chronic use.
- Ask for a blood test. Request a serum creatinine and eGFR test at your next checkup. If you’ve been on daily pain meds for over a year, you need this.
- Try one non-drug option. Start with heat therapy or a 15-minute daily walk. Small changes add up.
The FDA now requires kidney risk warnings on all NSAID packaging. But warnings don’t work if no one reads them. You have to be your own advocate. Your kidneys can’t speak up. But you can.
Why This Matters More Than You Think
Analgesic nephropathy causes 15,000 to 20,000 new cases of chronic kidney disease in the U.S. every year. That’s 2-3% of all cases. And it’s entirely preventable.
The cost? $18,500 per year for early-stage care. $90,000 if you need dialysis. That’s not just money-it’s time, energy, and quality of life lost.
And yet, a 2023 CDC report found that 41% of American adults still exceed recommended NSAID doses. Among people with chronic pain, that number jumps to 67%. We’re treating pain like a bug you spray away-not a signal your body is screaming.
There’s no magic pill. But there is a smarter way. Stop treating pain with constant chemical suppression. Start treating it with movement, heat, therapy, and targeted care. Your kidneys will thank you-for decades.
Can I still take ibuprofen if I have healthy kidneys?
Yes-but only occasionally and at low doses. Don’t take ibuprofen daily for more than 10 days without seeing a doctor. For chronic pain, the safest approach is to use the lowest effective dose for the shortest time possible. Even healthy kidneys can be damaged by long-term, high-dose use. Stick to 200-400 mg no more than 2-3 times a week, and never exceed 1,200 mg per day.
Is Tylenol (acetaminophen) safe for kidneys?
It’s safer than NSAIDs, but not risk-free. Taking more than 3,000 mg a day for several years increases your risk of chronic kidney disease by nearly 70%. The liver breaks down acetaminophen into toxins that stress the kidneys over time. If you’re using it daily, cut back. Try 2,000 mg or less per day, and never combine it with alcohol or other medications that affect the liver.
What are the early signs of kidney damage from painkillers?
There are usually no symptoms at first. That’s why it’s called silent damage. By the time you feel tired, swollen, or notice high blood pressure, the kidneys are already struggling. The only way to catch it early is through blood tests: rising creatinine and dropping eGFR. If you’ve been on daily painkillers for over a year, get tested. Don’t wait for symptoms.
Can analgesic nephropathy be reversed?
It can be stopped-and sometimes partially reversed-if caught early. Stopping all NSAIDs and acetaminophen is the first step. Studies show 73% of patients who stopped early had stable kidney function after five years. Once scarring sets in, it’s permanent. But halting further damage is still a huge win. The goal isn’t to cure the past-it’s to protect the future.
What pain relievers are safest for long-term use?
The safest options aren’t pills at all. Topical NSAID gels, heat therapy, physical therapy, and cognitive behavioral therapy offer effective pain relief without harming your kidneys. For nerve pain, duloxetine (Cymbalta) is a prescription option with no kidney risk. For migraines, CGRP inhibitors are safe but expensive. Always start with non-drug methods. If you need medication, use the lowest dose for the shortest time.
Are there new tests to detect kidney damage from painkillers?
Yes. In January 2023, the FDA approved NephroCheck, a point-of-care urine test that detects early signs of renal papillary damage. It’s 92% sensitive and can spot problems before creatinine rises. This is a game-changer for people on long-term pain meds. Ask your doctor if this test is available-it’s not yet routine, but it should be.
Final Thought: Pain Isn’t a Problem to Be Eliminated-It’s a Signal
Every time you pop a pill to silence pain, you’re ignoring a message. Your body is telling you something’s wrong-maybe inflammation, misalignment, stress, or nerve irritation. Painkillers don’t fix that. They just mute the alarm.
True healing comes from listening. From moving. From resting. From treating the cause, not just the symptom. Your kidneys don’t ask for much. Just don’t drown them in pills. Choose smarter. Choose safer. Choose your health.


And don’t even get me started on ‘acetaminophen is safe.’ That’s like saying a chainsaw is safe if you don’t turn it on. The damage is cumulative. Your liver doesn’t scream. Your kidneys don’t cry. They just… stop. Quietly. Like a factory worker who’s been underpaid for 30 years.
they banned phenacetin? sure. but they swapped it for ibuprofen and called it progress. laughable.
you want to feel better? stop being weak. go for a walk. lift something. stop whining. if you need a pill every day you’re not in pain you’re in laziness
my grandpa worked 12 hour shifts with a broken back and never took a pill. what’s your excuse?
in other countries, they treat pain like a medical issue. here? we treat it like a moral failure. if you’re on meds too long, you’re lazy. if you need therapy, you’re weak. if you need a CGRP inhibitor, you’re a rich snob.
we don’t fix systems. we shame people.
you don’t need to be pain-free to be healthy. you just need to stop poisoning yourself trying to erase the signal. start slow. one heat wrap a day. one 10-minute walk. you’ll be shocked how much better you feel without the chemical fog.
i’m switching to heat wraps and crying into my yoga mat. this post saved me. thank you. i’m not okay but i’m trying. 🙏
we treat discomfort like an enemy to be defeated, not a teacher to be listened to. the body speaks in signals. we respond with chemicals.
maybe the real question isn’t ‘what pill should i take?’ but ‘what is my body trying to tell me?’
heat, movement, rest - these aren’t alternatives. they’re the original medicine.
also i spell ibuprofen wrong like 80% of the time. sorry.
also the FDA is run by Pfizer bots. i saw it on a video. they have tails.