Tricyclic Antidepressants: What They Are, How They Work, and Alternatives
When you hear tricyclic antidepressants, a class of prescription medications first developed in the 1950s to treat depression by balancing brain chemicals like serotonin and norepinephrine. Also known as TCAs, they were the go-to treatment before SSRIs came along—but they’re not gone. Doctors still prescribe them for depression, chronic nerve pain, and sometimes for sleep or anxiety, especially when newer drugs don’t work.
These drugs work differently than today’s most common antidepressants. While SSRIs mostly boost serotonin, tricyclics hit both serotonin and norepinephrine, which can make them more effective for some people—especially those with physical symptoms like fatigue or pain. But that same power comes with trade-offs. Common side effects include dry mouth, drowsiness, weight gain, and blurred vision. In higher doses, they can affect heart rhythm, which is why doctors check your heart before and during treatment. They’re also dangerous in overdose, so they’re not usually the first choice for people with suicide risk.
That’s why many patients end up switching to newer options like SSRIs or SNRIs, which have fewer side effects and are safer in overdose. But not everyone responds to those. Some people find tricyclics work better for their depression or for conditions like fibromyalgia or migraine prevention. And because they’re generic, they’re often cheaper than brand-name alternatives. If you’ve tried other meds and still feel stuck, tricyclics might be worth discussing with your doctor—not because they’re the easiest choice, but because they’re one of the few that still work when others don’t.
What you’ll find below is a collection of real-world posts that connect to tricyclic antidepressants through related topics. You’ll see comparisons between older and newer antidepressants, discussions on managing side effects, and even how some of these drugs overlap with treatments for heart conditions, nerve pain, and sleep disorders. There’s no fluff here—just clear, practical info from people who’ve been there, doctors who’ve prescribed them, and studies that show what really works.
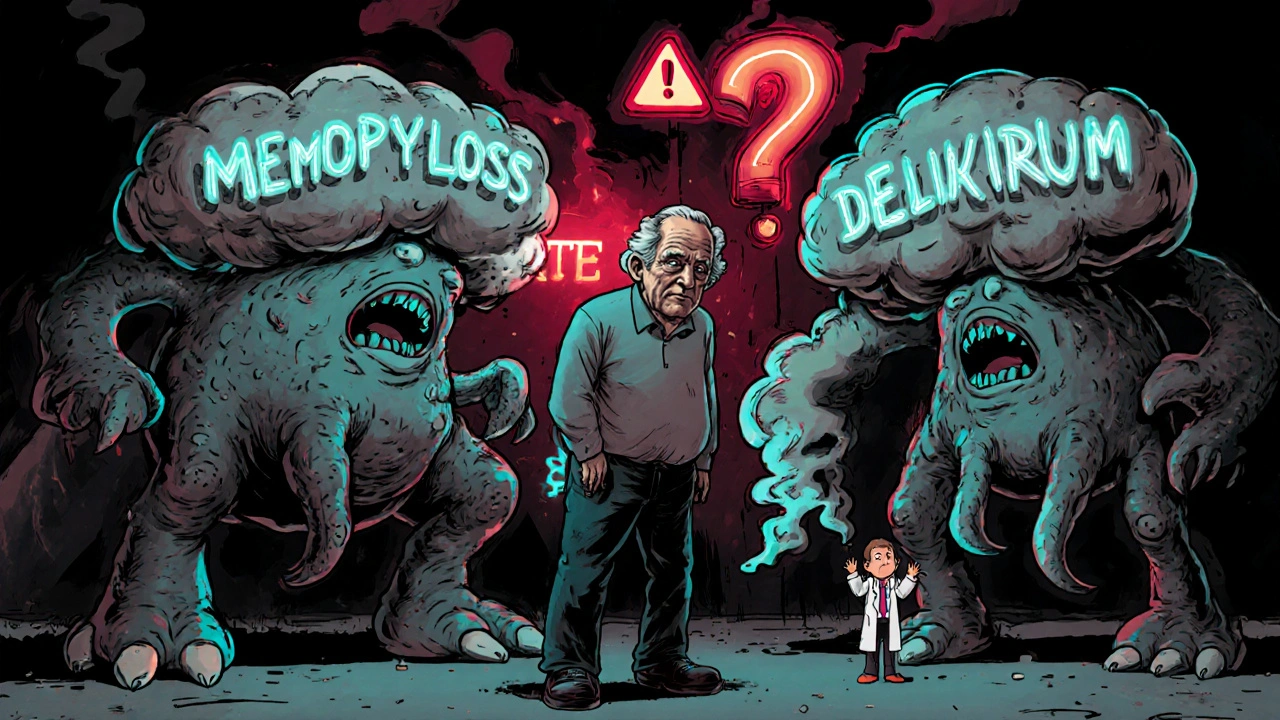
Tricyclic Antidepressants and Antihistamines: The Hidden Danger of Anticholinergic Overload
Combining tricyclic antidepressants like amitriptyline with first-gen antihistamines like Benadryl can cause dangerous anticholinergic overload, leading to confusion, delirium, and increased dementia risk-especially in older adults.