Ticlopidine: What It Is and When You Might Need It
If your doctor mentioned ticlopidine, you’re probably dealing with blood clot prevention. Ticlopidine is an antiplatelet drug that stops platelets from clumping together, which reduces the risk of strokes or heart attacks after certain procedures.
How Ticlopidine Works
The medicine blocks a receptor on platelets called P2Y12. By doing this, it interferes with the chemical signals that tell platelets to stick together. The result is smoother blood flow in arteries that might be narrowed by plaque.
Because it targets platelet activity directly, ticlopidine works slower than newer drugs like clopidogrel. You’ll usually start seeing its effect after a few days of regular dosing. That’s why doctors often prescribe a short loading dose followed by a maintenance schedule.
Tips for Safe Use
First off, follow the exact dosage your doctor gave you. The typical adult regimen is 250 mg twice daily for up to three weeks, then 250 mg once a day for long‑term use. Missed a dose? Take it as soon as you remember unless it’s almost time for the next one—don’t double up.
Watch out for common side effects: mild nausea, diarrhea, or headache can happen early on. More serious issues include low white‑blood‑cell counts (agranulocytosis) and liver problems. If you notice unusual bruising, fever, sore throat, or yellow skin, call your doctor right away.
Alcohol and certain antibiotics can boost ticlopidine levels in your blood, raising the risk of side effects. Always tell your pharmacist about other meds, supplements, or over‑the‑counter drugs you’re taking.
Pregnant or breastfeeding women should avoid ticlopidine unless a doctor says it’s absolutely necessary. The drug crosses the placenta and there isn’t enough safety data for newborns.
Finally, regular blood tests are part of the plan when you’re on ticlopidine. Your doctor will check your liver enzymes and white‑blood‑cell count every few weeks at first, then less often once everything looks stable.
In short, ticlopidine can be a solid choice for clot prevention, but it needs careful monitoring. Stick to the prescribed schedule, watch for side effects, and keep open communication with your healthcare team. That way you get the benefit of reduced clot risk without unexpected problems.
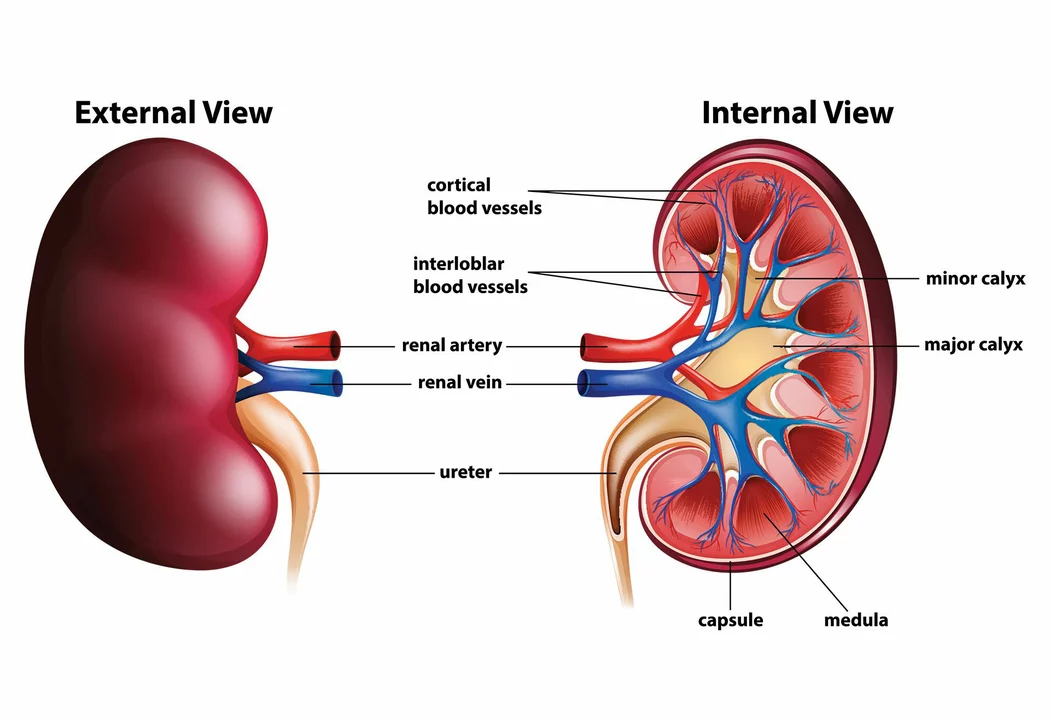
Ticlopidine and Renal Function: What You Need to Know
As a blogger, I recently researched the topic of Ticlopidine and its effects on renal function. Ticlopidine is an antiplatelet medication that is often prescribed to prevent blood clots, but it could potentially affect kidney function. It is essential to monitor renal function while taking this medication, as it may lead to complications. In some cases, doctors may adjust the dosage or consider alternative medications to ensure the safety of the patients. Overall, it is crucial to be aware of the potential impact of Ticlopidine on renal function and discuss any concerns with your healthcare provider.