Drug Effects: What They Are and Why You Should Care
Every pill you take does more than just treat a condition – it sends signals through your body that can help, hurt, or surprise you. Understanding those effects helps you stay safe, avoid nasty surprises, and get the most out of each medication.
Types of Drug Effects
The first thing to know is that drug effects come in three main flavors: therapeutic, side‑effects, and adverse reactions. Therapeutic effects are the good stuff – the relief from pain, lower blood pressure, or clearer skin you expect when you follow a prescription.
Side‑effects are the not‑so‑great but often predictable outcomes, like mild nausea from antibiotics or drowsiness after antihistamines. They’re usually short‑lived and manageable.
Adverse reactions are the scary ones – unexpected, severe, or life‑threatening responses such as an allergic rash, liver damage, or a sudden drop in heart rate. These can happen even if you’ve taken the drug before without trouble.
What decides which effect shows up? Dosage is a big player: too much raises the risk of both side‑effects and adverse events. Age, weight, genetics, kidney function, and other meds you’re on also shape how your body reacts.
Tips for Managing Drug Effects
First, keep a simple log. Write down what you take, when you take it, and any new feeling that pops up. A quick note on your phone can reveal patterns you might otherwise miss.
Second, never skip the label. Dosage instructions, food warnings, and timing cues are there for a reason. If something says “take with food,” doing the opposite can crank up stomach irritation.
Third, talk to your pharmacist or doctor as soon as you notice anything odd. Even mild symptoms can hint at an interaction that needs adjusting. A short call can prevent a bigger problem down the road.
Fourth, watch out for drug‑drug interactions. Mixing over‑the‑counter pain relievers with certain blood thinners, for example, can boost bleeding risk. Use one pharmacy if you can – they’ll see all your prescriptions in one place.
Finally, consider personal factors. If you’re older or have kidney disease, ask whether a lower dose might work just as well. Genetics play a role too; some people metabolize drugs faster, meaning they need higher doses for the same effect.
Remember, feeling a new symptom doesn’t always mean the drug is bad. It could be your body adjusting, especially with antidepressants or blood pressure meds that take weeks to settle. Patience combined with monitoring usually does the trick.
If you ever suspect an allergic reaction – swelling, trouble breathing, or a rash that spreads quickly – treat it as an emergency. Call 911 or get to an ER right away; time matters.
Bottom line: drug effects are a two‑way street. You control part of the journey by following instructions, tracking changes, and staying in touch with your healthcare team. By doing so, you keep the good benefits rolling while keeping risks low.
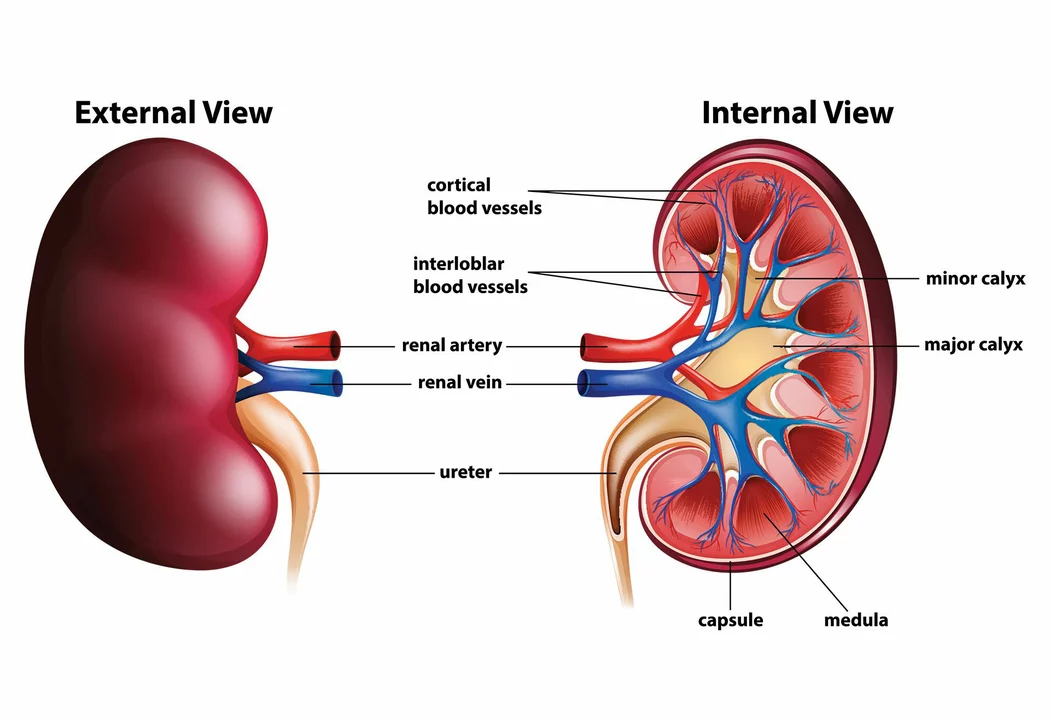
Ticlopidine and Renal Function: What You Need to Know
As a blogger, I recently researched the topic of Ticlopidine and its effects on renal function. Ticlopidine is an antiplatelet medication that is often prescribed to prevent blood clots, but it could potentially affect kidney function. It is essential to monitor renal function while taking this medication, as it may lead to complications. In some cases, doctors may adjust the dosage or consider alternative medications to ensure the safety of the patients. Overall, it is crucial to be aware of the potential impact of Ticlopidine on renal function and discuss any concerns with your healthcare provider.