Diphenhydramine: What It Is, How It Works, and What Else You Should Know
When you reach for something to help with allergies, a stuffy nose, or trouble falling asleep, you might grab a bottle of diphenhydramine, a first-generation antihistamine that blocks histamine receptors to reduce allergy symptoms and cause drowsiness. Also known as Benadryl, it’s one of the most recognizable names in over-the-counter medicine. But diphenhydramine isn’t just for sneezing fits—it’s also used for motion sickness, coughs, and even as a sleep aid. The catch? It doesn’t just calm your nose. It slows down your brain, which is why you feel so tired after taking it.
That drowsiness? It’s not a bug—it’s a feature. Diphenhydramine crosses the blood-brain barrier easily, which is why it’s so effective at making you sleepy. But it also means side effects like dry mouth, blurry vision, and confusion can happen, especially in older adults. That’s why doctors often recommend newer antihistamines like loratadine or cetirizine for daily allergy use—they work just as well without the foggy head. But if you need something strong to knock you out at night, diphenhydramine still holds its ground. It’s also used off-label for mild anxiety, tremors, and even some movement disorders related to Parkinson’s or medication side effects.
What’s interesting is how often diphenhydramine shows up in other medicines. You’ll find it in nighttime cold formulas, sleep gels, and even some combination pain relievers. But stacking it with alcohol, other sedatives, or even certain antidepressants can be risky. It’s not just about drowsiness—it’s about how your body handles the chemical load. And while it’s available without a prescription, that doesn’t mean it’s harmless. Long-term use, especially for sleep, can lead to tolerance, dependence, or even cognitive decline in older people.
That’s why the posts below cover more than just diphenhydramine itself. You’ll find comparisons with other antihistamines, discussions on how they affect eczema itch, warnings about mixing them with other drugs, and even how some of these same sedating agents show up in unexpected places like cough syrups or motion sickness patches. Whether you’re using it for allergies, sleep, or just to get through a bad night, knowing what else is in your medicine cabinet—and what might be interacting with it—could make all the difference.
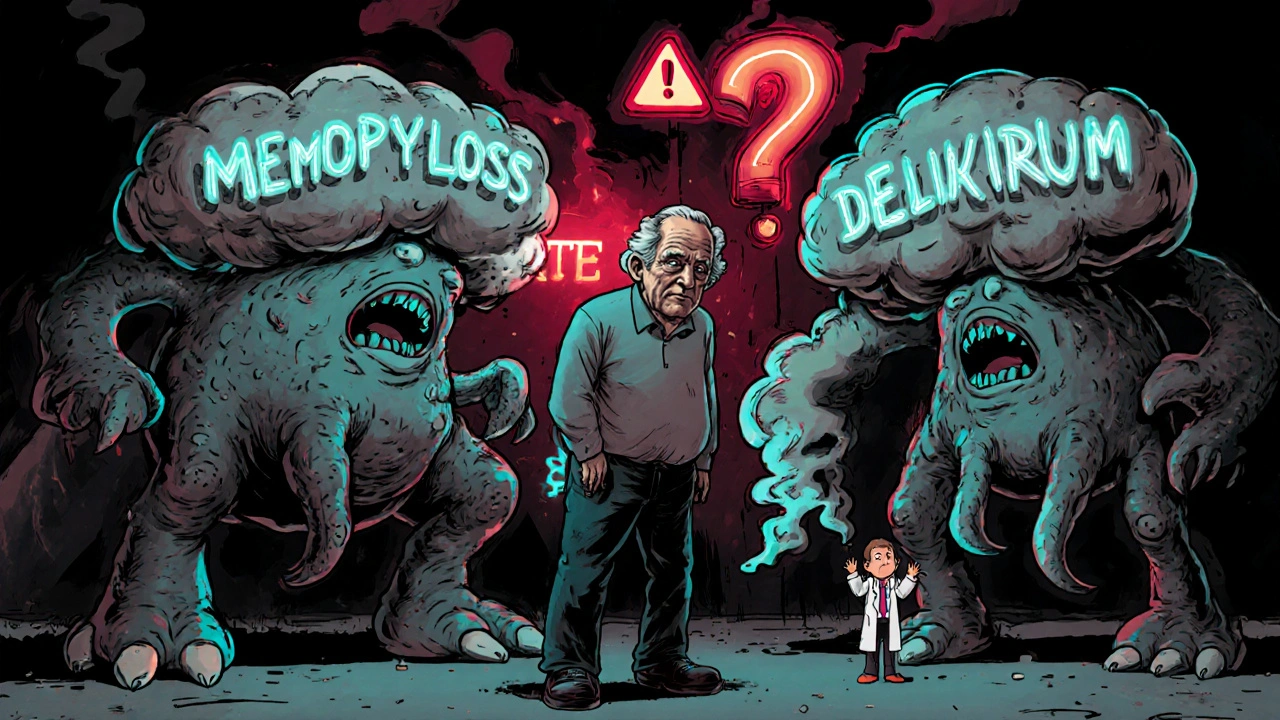
Tricyclic Antidepressants and Antihistamines: The Hidden Danger of Anticholinergic Overload
Combining tricyclic antidepressants like amitriptyline with first-gen antihistamines like Benadryl can cause dangerous anticholinergic overload, leading to confusion, delirium, and increased dementia risk-especially in older adults.