Beta-Blockers and Asthma: Risks, Alternatives, and Safe Choices
When you have beta-blockers, a class of medications used to lower blood pressure, slow heart rate, and treat heart conditions. Also known as beta-adrenergic blocking agents, they work by blocking adrenaline’s effects on the heart and blood vessels. But for people with asthma, a chronic lung condition that causes airway narrowing, wheezing, and shortness of breath, these drugs can be risky. Why? Because beta-blockers can cause bronchoconstriction, the tightening of airways in the lungs that makes breathing harder—exactly what asthma patients are trying to avoid.
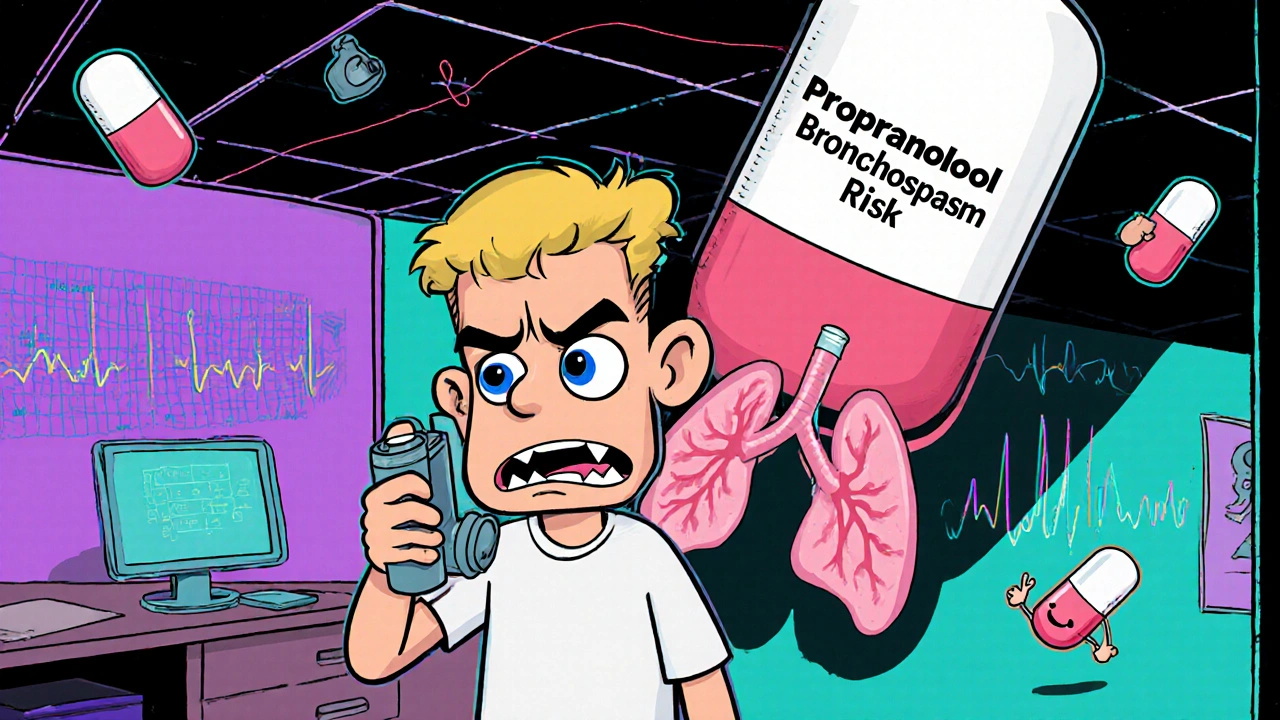
Not all beta-blockers are the same. Some, like propranolol, block both beta-1 and beta-2 receptors. Beta-2 receptors are found in the lungs and help keep airways open. Blocking them can trigger an asthma attack. Even if you’ve never had a problem before, a sudden illness or stress can make your airways more sensitive. That’s why many doctors avoid prescribing non-selective beta-blockers to asthma patients altogether. But what if you also have high blood pressure or heart disease? You can’t just stop treating your heart. That’s where selective beta-blockers come in—drugs like metoprolol or atenolol that mostly target the heart and have less effect on the lungs. Still, even these aren’t risk-free. Your doctor will weigh the benefits against the chance of worsening breathing, and they’ll likely start you on the lowest possible dose while watching your symptoms closely.
There are other options. If you’re on a beta-blocker because of heart failure or arrhythmia, your doctor might switch you to a different type of medication—like calcium channel blockers, ACE inhibitors, or ARBs—that don’t touch your airways. For asthma patients with high blood pressure, these alternatives often work just as well without the danger. And if you’re using a beta-blocker for migraines or anxiety, there are non-beta-blocker treatments available too. The key is communication. Tell your doctor you have asthma before they write any new prescription. Bring a list of everything you’re taking, including over-the-counter meds. Some cold remedies and decongestants can also tighten airways, so even small choices matter.
The posts below dive into real-world cases and alternatives you might not know about. You’ll find comparisons of heart medications that are safer for asthma, warnings about hidden triggers in common drugs, and practical tips for managing multiple conditions without putting your breathing at risk. Whether you’re a patient, caregiver, or just trying to understand why your doctor changed your prescription, this collection gives you clear, no-fluff answers.
Beta-Blockers and Asthma: What You Need to Know About Bronchospasm Risks and Safer Choices
Beta-blockers were once banned for asthma patients due to bronchospasm risks. New evidence shows cardioselective options like atenolol and bisoprolol are safe for many, offering heart protection without triggering asthma attacks.