Atenolol for Asthma: Why It's Risky and What to Use Instead
When you have asthma, a chronic lung condition that causes airway narrowing, wheezing, and trouble breathing. Also known as reactive airway disease, it requires careful medication choices to avoid triggering attacks. One of the most dangerous mistakes is using atenolol, a beta-blocker commonly prescribed for high blood pressure and heart rhythm issues. Also known as Tenormin, it can shut down the airways in people with asthma, leading to life-threatening bronchoconstriction. Even low doses can make breathing harder, and many patients don’t realize the risk until they’re in distress.
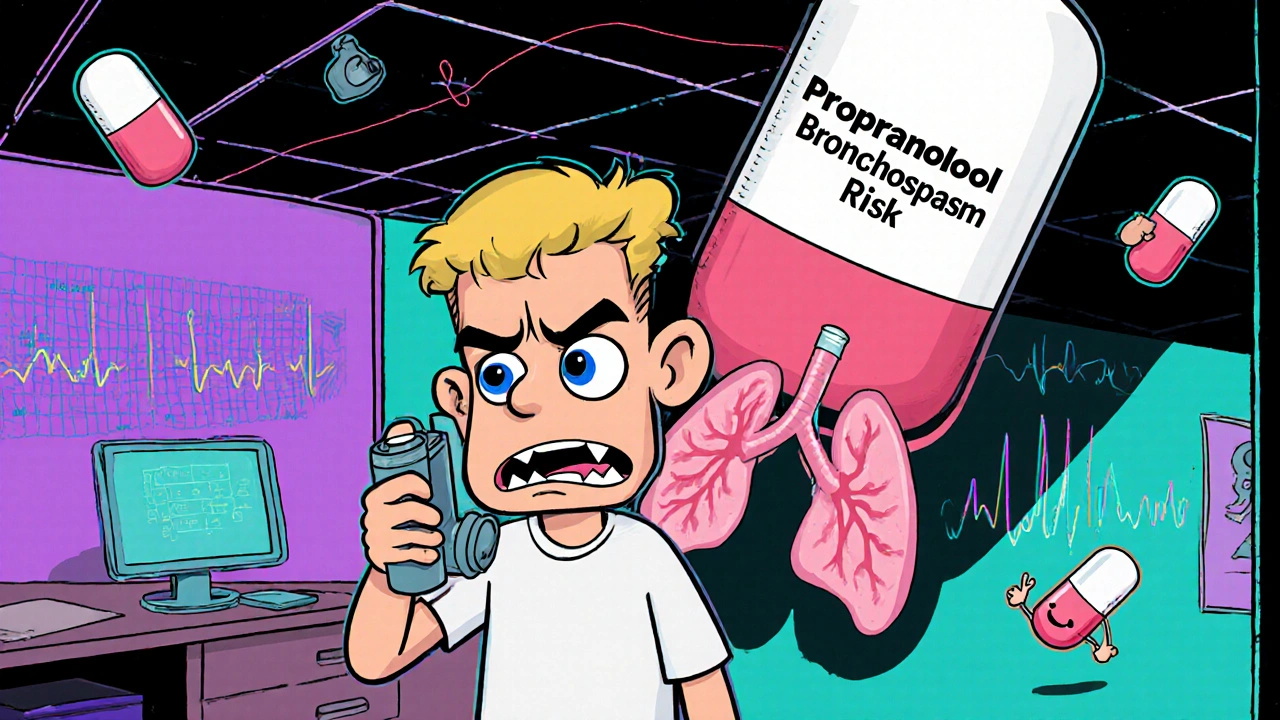
Atenolol blocks beta receptors in the heart to slow the pulse and lower blood pressure—but it also blocks those same receptors in the lungs. That’s bad news for asthmatics. Beta-2 receptors in the airways help keep them open. When atenolol blocks them, the muscles around the airways tighten, causing wheezing, coughing, and sometimes full-blown asthma attacks. Studies from the American Thoracic Society show that non-selective beta-blockers like propranolol are especially risky, but even cardioselective ones like atenolol aren’t safe for long-term use in asthma patients. The FDA has issued warnings about this for decades, yet some doctors still prescribe it, especially if they don’t know the patient’s full history.
So what’s the alternative? If you have both high blood pressure and asthma, there are safer options. Calcium channel blockers like amlodipine or diltiazem work just as well for blood pressure without touching the lungs. ACE inhibitors like lisinopril are another solid choice. For heart rate control, doctors might turn to non-beta-blocker options like ivabradine. And if you absolutely need a beta-blocker, some newer ones like bisoprolol may be used cautiously under strict supervision—but never as a first-line treatment.
You might be wondering, "Why do some people still get prescribed atenolol?" Often, it’s because their asthma wasn’t diagnosed yet, or their doctor assumed their symptoms were just anxiety. Or maybe they were prescribed it for a heart condition before asthma showed up. That’s why it’s critical to tell every provider you see that you have asthma—no matter how mild it seems. A simple note in your chart can prevent a serious reaction.
The posts below dive into other medications that can clash with asthma, from clenbuterol misuse to how antihistamines affect breathing, and what to take instead when your heart and lungs are both in play. You’ll find real comparisons, safety tips, and clear alternatives—no jargon, no fluff. Just what you need to stay safe and in control.
Beta-Blockers and Asthma: What You Need to Know About Bronchospasm Risks and Safer Choices
Beta-blockers were once banned for asthma patients due to bronchospasm risks. New evidence shows cardioselective options like atenolol and bisoprolol are safe for many, offering heart protection without triggering asthma attacks.