Amitriptyline: Uses, Side Effects, and Alternatives for Depression and Chronic Pain
When you hear amitriptyline, a tricyclic antidepressant originally developed in the 1960s for depression but now widely used for nerve pain and sleep disorders. Also known as Elavil, it’s one of the most prescribed drugs in its class, even today, despite newer options. It doesn’t just lift mood—it changes how your brain processes pain signals, which is why doctors give it for conditions like fibromyalgia, diabetic neuropathy, and chronic headaches, not just sadness.
What makes amitriptyline different from SSRIs like Celexa or Prozac? It hits more than one neurotransmitter. It boosts serotonin and norepinephrine, which helps with both mood and pain. But that also means more side effects—dry mouth, drowsiness, weight gain, and sometimes dizziness when standing up. People often stop taking it because of these, not because it doesn’t work. That’s why many switch to gabapentin, a nerve pain medication with fewer systemic side effects, or duloxetine, an SNRI that’s FDA-approved for both depression and chronic pain. Both are gentler on the body but might not work as well for everyone.
If you’ve been on amitriptyline for a while and feel stuck, you’re not alone. Many patients use it long-term because their doctor never discussed alternatives. But there are options: low-dose nortriptyline (a metabolite of amitriptyline with fewer side effects), topical lidocaine patches for localized pain, or even non-drug approaches like CBT for chronic pain management. Even though it’s old, amitriptyline still has a place—especially for people who don’t respond to newer drugs or need help sleeping along with their pain. But it’s not a one-size-fits-all solution.
What you’ll find below are real comparisons and experiences from people who’ve used amitriptyline—some for depression, others for back pain or migraines. You’ll see how it stacks up against other meds, what side effects really look like in practice, and which alternatives actually helped when amitriptyline didn’t. No fluff. Just what works, what doesn’t, and what to ask your doctor next.
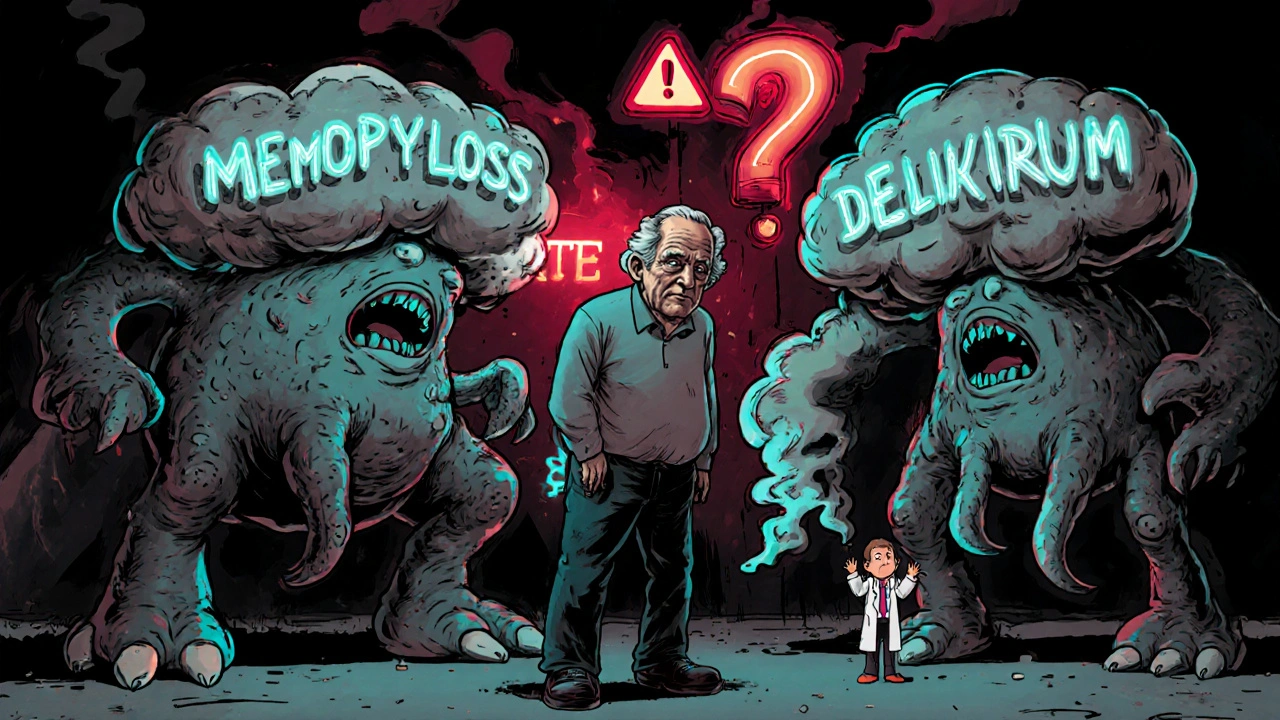
Tricyclic Antidepressants and Antihistamines: The Hidden Danger of Anticholinergic Overload
Combining tricyclic antidepressants like amitriptyline with first-gen antihistamines like Benadryl can cause dangerous anticholinergic overload, leading to confusion, delirium, and increased dementia risk-especially in older adults.